Correlation Between Energy Spectrum CT Iodine-Based Values and FEV1/FVC in Early-Stage Small Airway Damage of the Lung
-
摘要:
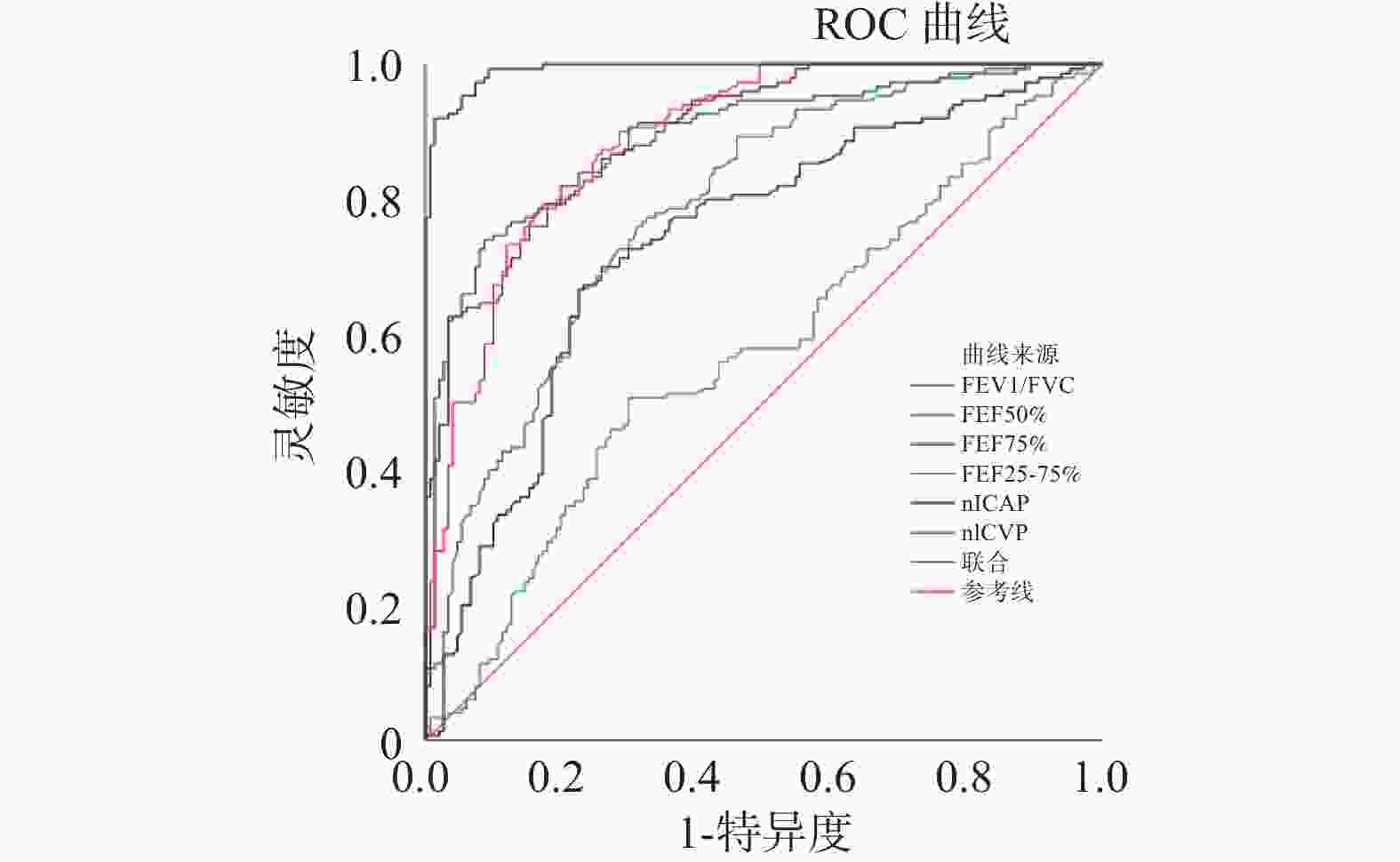
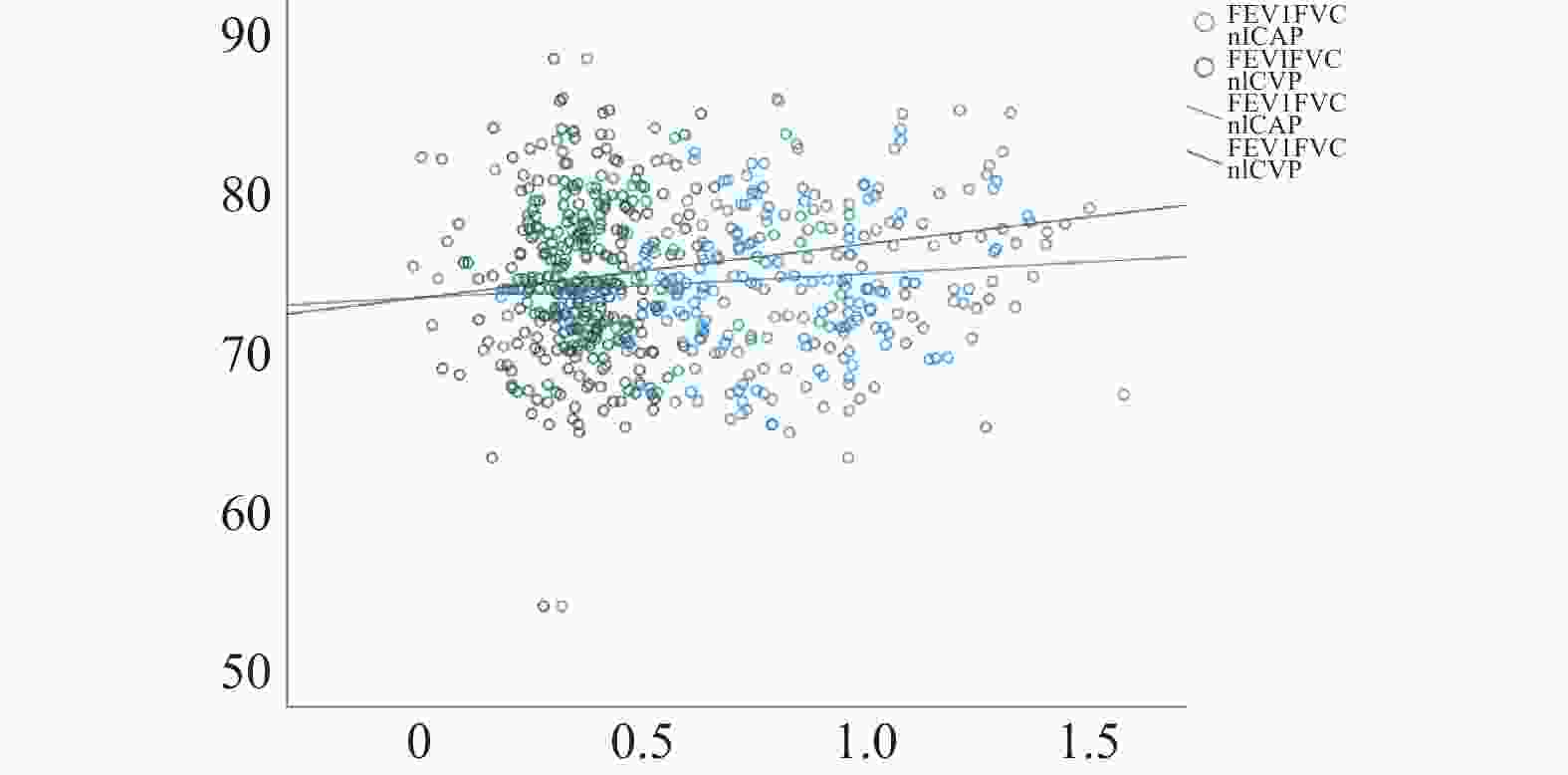
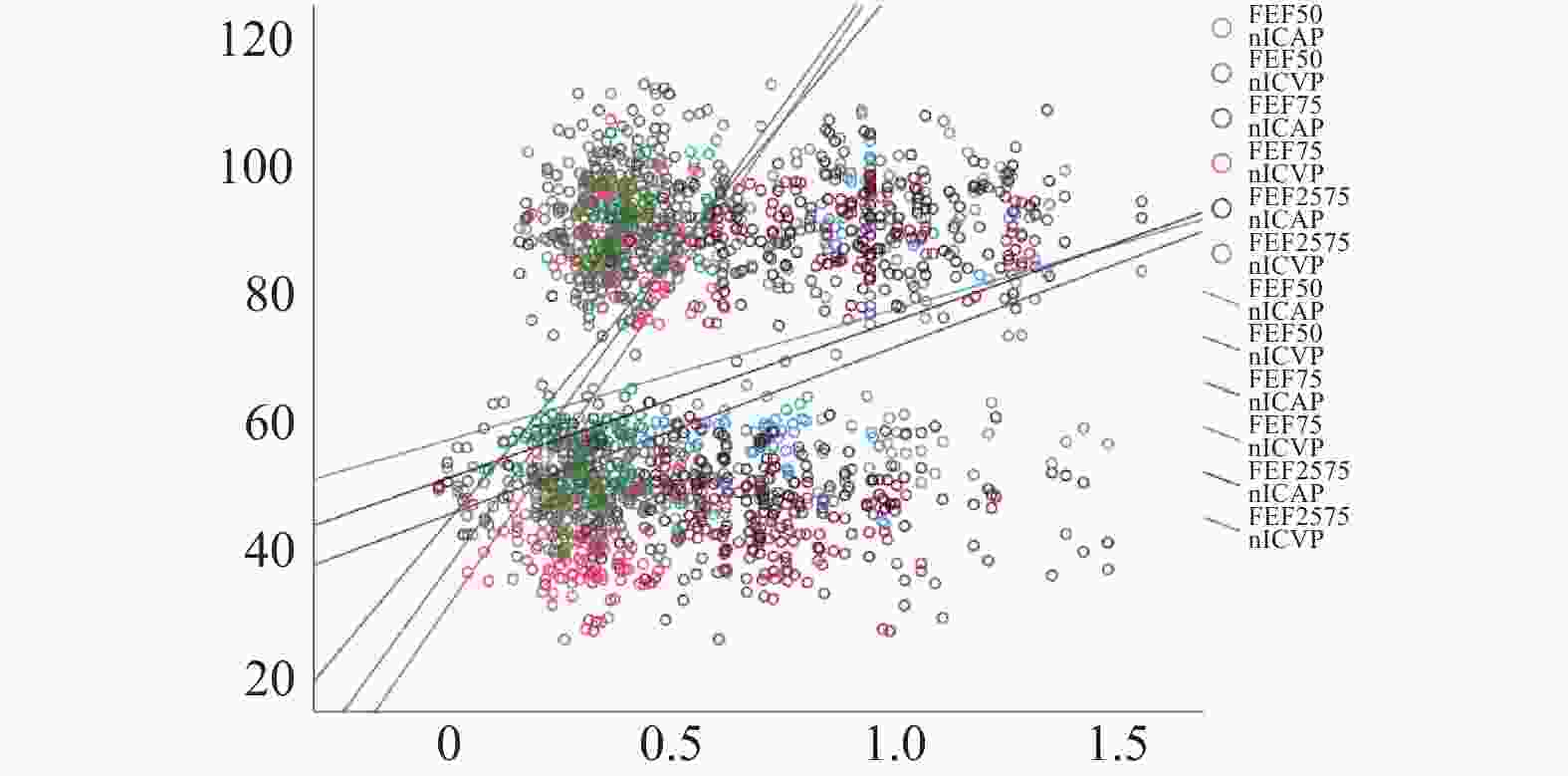
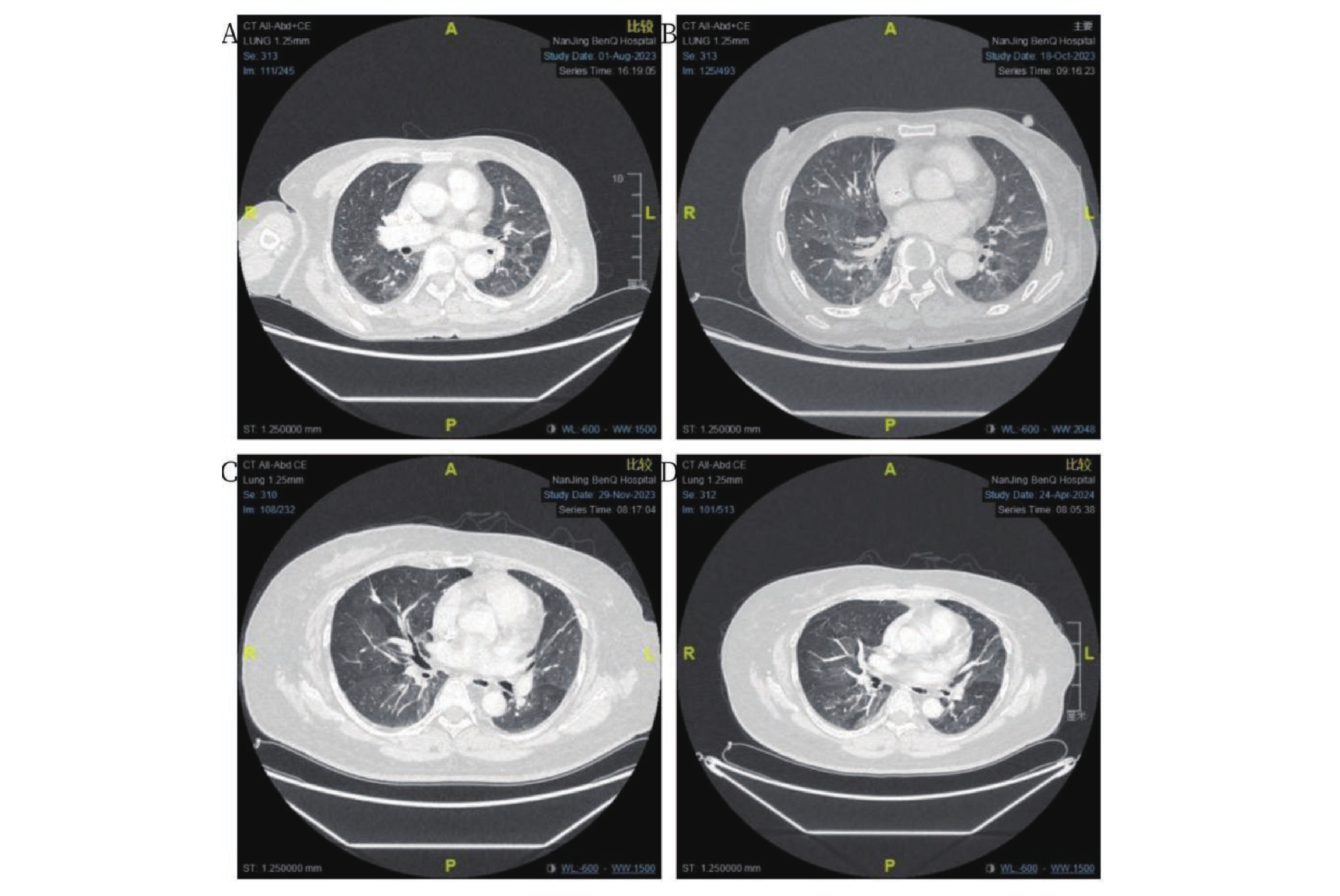
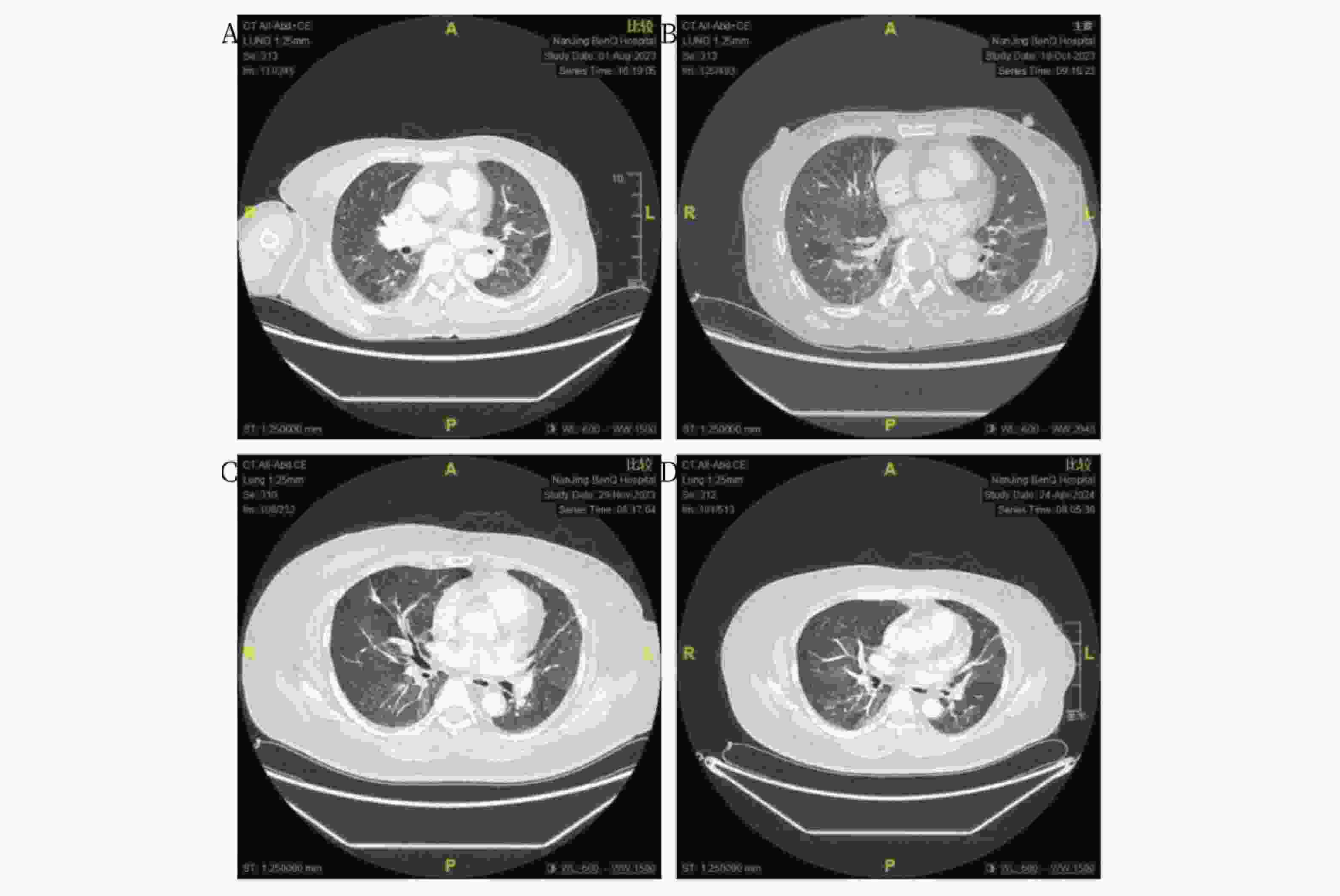
目的 探讨肺小气道损害患者能谱CT碘基值与肺通气功能参数的关系。 方法 回顾性分析2021年8月至2024年12月南京明基医院收治的152例早期肺小气道损害患者临床资料,作为观察组;另收集同期在医院健康体检者152例临床资料,作为对照组。所有受检者资料均完整,包括能谱CT检查资料、肺功能检查资料及一般资料。比较两组的能谱CT检查参数及肺功能参数,分析能谱CT碘基值筛查早期肺小气道损害的价值,并分析肺小气道损害患者能谱CT碘基值与第1秒用力呼气容积(forced expiratory volume in one second,FEV1)/用力肺活量(forced vital capacity,FVC)的相关性。 结果 观察组FEV1/FVC、FEF50%、FEF75%、FEF25%~75%均比对照组低(P < 0.05);观察组能谱CT的动脉期标准化碘基值(normalized iodine concentration in arterial phase,nICAP)、静脉期标准化碘基值(normalized iodine concentration in venous phase,nICVP)值均比对照组低(P < 0.05);经Logistic回归分析发现,FEV1/FVC、FEF50%、FEF75%、FEF25%~75%、nICAP、nICVP升高均是早期肺小气道损害的保护因子(OR < 1,P < 0.05);ROC曲线结果显示,能谱CT nICAP、nICVP值及FEV1/FVC、FEF50%、FEF75%、FEF25%~75%筛查早期肺小气道损害的AUC均>0.50,且联合筛查早期肺小气道损害的AUC>0.90,筛查价值较高;采用双变量Pearson直线相关性分析结果显示,早期肺小气道损害患者FEV1/FVC与nICAP、nICVP之间无相关性(r = 0.096、0.076,P = 0.098、0.189),与FEF50%、FEF75%、FEF%25~75%之间呈正相关(P < 0.05)。 结论 能谱CT碘基值与肺小气道损害存在相关性,而早期肺小气道损害患者的能谱CT碘基值与FEV1/FVC之间无相关性。 Abstract:Objective To investigate the relationship between spectral computed tomography (CT) iodine-based values and pulmonary ventilation function parameters in patients with early-stage pulmonary small airway dysfunction. Methods A retrospective analysis was conducted on the clinical data of 152 patients with early-stage pulmonary small airway dysfunction admitted to Nanjing Mingji Hospital from August 2021 to December 2024, designated as the observation group. Additionally, 152 cases of clinical data from healthy individuals who underwent physical examination at the hospital during the same period were collected as the control group. All subjects had complete data including spectral CT imaging data, pulmonary function test data, and general information. Spectral CT parameters and pulmonary function parameters between the two groups were compared. The value of spectral CT iodine-based values in screening for early-stage pulmonary small airway dysfunction was analyzed, and the correlation between spectral CT iodine-based values and forced expiratory volume in one second (FEV1)/forced vital capacity (FVC) in patients with pulmonary small airway dysfunction was examined. Results FEV1/FVC, FEF50%, FEF75%, and FEF25%~75% in the observation group were significantly lower than those in the control group (P < 0.05). Normalized iodine concentration in arterial phase (nICAP) and normalized iodine concentration in venous phase (nICVP) values on spectral CT in the observation group were significantly lower than those in the control group (P < 0.05). Logistic regression analysis revealed that increases in FEV1/FVC, FEF50%, FEF75%, FEF25%~75%, nICAP, and nICVP were all protective factors against early-stage pulmonary small airway dysfunction (OR < 1, P < 0.05). ROC curve analysis demonstrated that the area under the curve (AUC) for spectral CT nICAP and nICVP values and FEV1/FVC, FEF50%, FEF75%, FEF25%~75% in screening for early-stage pulmonary small airway dysfunction were all greater than 0.50, with combined screening achieving an AUC greater than 0.90, indicating high screening value. Bivariate Pearson linear correlation analysis showed no correlation between FEV1/FVC and nICAP and nICVP in patients with early-stage pulmonary small airway dysfunction (r = 0.096, 0.076; P = 0.098, 0.189), while positive correlations were found with FEF50%, FEF75%, and FEF25%~75% (P < 0.05). Conclusion Spectral CT iodine-based values are correlated with pulmonary small airway dysfunction; however, no correlation exists between spectral CT iodine-based values and FEV1/FVC in patients with early-stage pulmonary small airway dysfunction. -
表 1 两组一般资料比较[n(%)/($ \bar x \pm s $)]
Table 1. Comparison of general information between two groups[n(%)/($ \bar x \pm s $)]
组别 性别 年龄(岁) 体重指数(kg/m2) 合并高血压 合并糖尿病 男 女 对照组(n = 152) 78(51.32) 74(48.68) 48.10 ± 6.39 23.20 ± 1.74 25(16.45) 17(11.18) 观察组(n = 152) 80(52.63) 72(47.37) 47.86 ± 6.12 23.12 ± 1.88 23(15.13) 15(9.87) χ2/t 0.053 0.334 0.385 0.099 0.140 P 0.818 0.738 0.701 0.753 0.709 表 2 两组FEV1/FVC、FEF50%、FEF75%、FEF25%~75%比较($ \bar x \pm s $)
Table 2. Comparison of FEV1/FVC,FEF50%,FEF75%,and FEF25%~75% between two groups($ \bar x \pm s $)
组别 n FEV1/FVC(%) FEF50% FEF75% FEF25%~75% 对照组 152 75.35 ± 4.73 92.13 ± 8.57 89.73 ± 7.29 91.35 ± 6.64 观察组 152 73.88 ± 4.69 54.35 ± 5.20 42.38 ± 6.71 49.73 ± 5.54 t 2.721 46.466 58.919 58.337 P 0.007* <0.001* <0.001* <0.001* *P < 0.05。 表 3 两组nICAP、nICVP值比较($ \bar x \pm s $)
Table 3. Comparison of nICAP and nICVP values between two groups($ \bar x \pm s $)
组别 n nICAP nICVP 对照组 152 0.95 ± 0.32 0.39 ± 0.10 观察组 152 0.65 ± 0.31 0.31 ± 0.11 t 8.302 6.635 P <0.001* <0.001* *P < 0.05。 表 4 各指标与早期肺小气道损害关系的Logistic回归分析
Table 4. Logistic regression analysis of the relationship between each index and early pulmonary small airway damage
项目 B S.E. Walsχ2 P OR 95%CI 常量 −83.435 21.607 14.911 <0.001* − − FEV1/FVC −0.094 0.047 3.946 0.047* 0.910 0.829~0.999 FEF50% −0.303 0.075 16.344 <0.001* 0.739 0.638~0.856 FEF75% −0.289 0.079 13.273 <0.001* 0.749 0.641~0.875 FEF25%~75% −0.345 0.077 20.324 <0.001* 0.708 0.609~0.823 nICAP −3.046 0.631 23.312 <0.001* 0.048 0.014~0.164 nICVP −8.197 1.912 18.380 <0.001* 0.000 0.000~0.012 *P < 0.05。 表 5 能谱CT碘基值、肺功能指标筛查早期肺小气道损害价值分析结果
Table 5. Value of energy spectrum CT iodine baseline values and lung function indicators in screening early pulmonary small airway damage
变量 AUC AUC 95%CI cut-off值 P 特异度 灵敏度 约登指数 FEV1/FVC 0.574 0.509~0.639 74.635% 0.026* 0.580 0.520 0.100 FEF50% 0.894 0.858~0.930 86.000 <0.001* 0.853 0.773 0.626 FEF75% 0.895 0.861~0.930 82.945 <0.001* 0.800 0.800 0.600 FEF25-75% 0.891 0.855~0.926 85.595 <0.001* 0.803 0.800 0.603 nICAP 0.737 0.680~0.794 0.812 <0.001* 0.740 0.700 0.440 nICVP 0.787 0.737~0.838 0.323 <0.001* 0.700 0.740 0.440 联合 0.993 0.987~0.998 − <0.001* 0.827 0.993 0.820 *P < 0.05。 表 6 相关性分析结果
Table 6. Correlation analysis results
指标 nICAP nICVP r P r P FEF50% 0.293 <0.001* 0.445 <0.001* FEF75% 0.309 <0.001* 0.442 <0.001* FEF25%~75% 0.330 <0.001* 0.479 <0.001* *P < 0.05。 -
[1] 黄晓旗, 牛媛, 雷禹, 等. 基于CT双气相定量研究吸烟合并慢性阻塞性肺疾病患者的肺叶小气道病变及肺气肿损伤程度[J]. 中华放射学杂志, 2022, 56(5): 536-541. doi: 10.3760/cma.j.cn112149-20210428-00418 [2] Qu Y, Wang L, Liu J. Evaluating the clinical utility of small airway function assessment for early diagnosis of GOLD stage 0 chronic obstructive pulmonary disease[J]. J Asthma, 2024, 61(11): 1554-1560. doi: 10.1080/02770903.2024.2368178 [3] Zhang D, Guan Y, Zhou X, et al. Aerodynamic simulation of small airway resistance: A new imaging biomarker for chronic obstructive pulmonary disease[J]. Int J Chron Obstruct Pulmon Dis, 2024, 19: 1167-1175. doi: 10.2147/COPD.S456878 [4] 蒋萍影, 唐国英. 外周血EETs水平与咳嗽变异性哮喘患儿Th1和Th2及其细胞因子、小气道功能的相关性分析[J]. 中国妇幼健康研究, 2024, 35(2): 38-43. doi: 10.3969/j.issn.1673-5293.2024.02.006 [5] 陈宏志, 朱林, 郭飞. 能谱CT低灌注在急性肺动脉栓塞风险分层中的应用[J]. 蚌埠医学院学报, 2024, 49(1): 103-105+109. doi: 10.13898/j.cnki.issn.1000-2200.2024.01.023 [6] 朱林, 卢冉, 郭飞. 能谱CT全肺平均灌注碘基值对急性肺动脉栓塞危险分层的效果评估[J]. 国际医学放射学杂志, 2022, 45(5): 503-507. doi: 10.19300/j.2022.L19393 [7] Ling K M, Garratt L W, Banerjee B, et al. Azithromycin partially mitigates dysregulated repair of lung allograft small airway epithelium[J]. Transplantation, 2020, 104(6): 1166-1176. doi: 10.1097/TP.0000000000003134 [8] Xu W J, Shang W Y, Feng J M, et al. Machine learning for accurate detection of small airway dysfunction-related respiratory changes: An observational study[J]. Respir Res, 2024, 25(1): 286. doi: 10.1186/s12931-024-02911-1 [9] 孙天生, 宋慧慧, 唐昊. 小气道功能在支气管哮喘中的研究进展[J]. 临床肺科杂志, 2024, 29(5): 754-758. doi: 10.3969/j.issn.1009-6663.2024.05.020 [10] Bai H, Shi C, Yu S, et al. A comparative study on the value of lower airway exhaled nitric oxide combined with small airway parameters for diagnosing cough-variant asthma[J]. Ther Adv Respir Dis, 2023, 17: 17534666231181259. [11] 牛媛, 雷禹, 沈敏, 等. 基于双气相配准定量CT评估COPD患者小气道病变[J]. 放射学实践, 2022, 37(12): 1516-1522. doi: 10.13609/j.cnki.1000-0313.2022.12.010 [12] 解宝珠, 丁琦, 李华, 等. 慢性阻塞性肺疾病小气道病变检测技术的研究进展[J]. 医学综述, 2023, 29(4): 730-736. [13] Lu L, Wu F, Tang G, et al. Associations of small airway dysfunction assessed by impulse oscillometry with lung function decline and exacerbations in participants with chronic obstructive pulmonary disease: A prospective cohort study in China[J]. Respir Med, 2025, 241: 108075. doi: 10.1016/j.rmed.2025.108075 [14] 赵凡惠, 王雷, 朱彦瑾, 等. 基于双气相定量CT评估COPD患者小气道病变和肺气肿程度的研究[J]. 临床放射学杂志, 2019, 38(12): 2307-2312 doi: 10.13437/j.cnki.jcr.2019.12.019 [15] 刘霞, 郭丹丹, 李春平, 等. HRCT肺小血管面积定量测量与COPD小气道功能的相关性研究[J]. 医学影像学杂志, 2022, 32(2): 240-245. doi: 10.20258/j.cnki.1006-9011.2022.02.014 [16] 崔可慧, 苏新明. 呼出气一氧化氮检测与稳定期慢性阻塞性肺疾病患者小气道改变及预后的相关性[J]. 中国医科大学学报, 2023, 52(1): 12-17. doi: 10.12007/j.issn.0258-4646.2023.01.003 [17] Meng X W, Pi Y W, Wang G L, et al. The relationship between quantitative parameters of dual-energy CT and HIF-1α expression in non-small cell lung cancer[J]. Curr Med Imaging, 2024, 20: e15734056271811. [18] 赵岩, 汤林花, 徐润桃, 等. 急性肺栓塞双能量能谱CT碘基物质图联合肺灌注缺损指数的运用价值[J]. 医学影像学杂志, 2023, 33(9): 1581-1584. [19] 贾艳荣, 张凤翔, 张芳, 等. 能谱CT联合MRI-DWI在鉴别肺炎性结节与肺癌中的价值[J]. 医学影像学杂志, 2024, 34(11): 57-61. [20] Alomari M, Wadiwala I, Bowers S , et al. Oxygen saturation endoscopic imaging as a novel alternative to assess tissue perfusion during esophagectomy[J]. Surg Innov, 2024, 31(6): 622-626. [21] 肖慧娟, 刘谊和, 梁盼, 等. Revolution 256 CT低剂量能谱碘水基物质对及三段能谱曲线斜率法定量鉴别不同周围型肺癌[J]. 医学影像学杂志, 2024, 34(4): 28-32. [22] Jiang D, Qin L, Pan W, et al. The value of high-pitch scanning with Sn100kV and ADMIRE in CT examination of tuberculous destroyed lung: Identifying the optimal combination for ultra-low-dose imaging[J]. PLoS One, 2025, 20(5): e0322374. doi: 10.1371/journal.pone.0322374 [23] Bodenberger A L, Konietzke P, Weinheimer O, 等. 气道壁能谱CT单能虚拟对比增强的定量研究[J]. 国际医学放射学杂志, 2023, 46(5): 626. -





 下载:
下载: