Risk Factors for Primary Aldosteronism in a Hypertensive Population Predicted by Logistic Regression and Decision Tree Models
-
摘要:
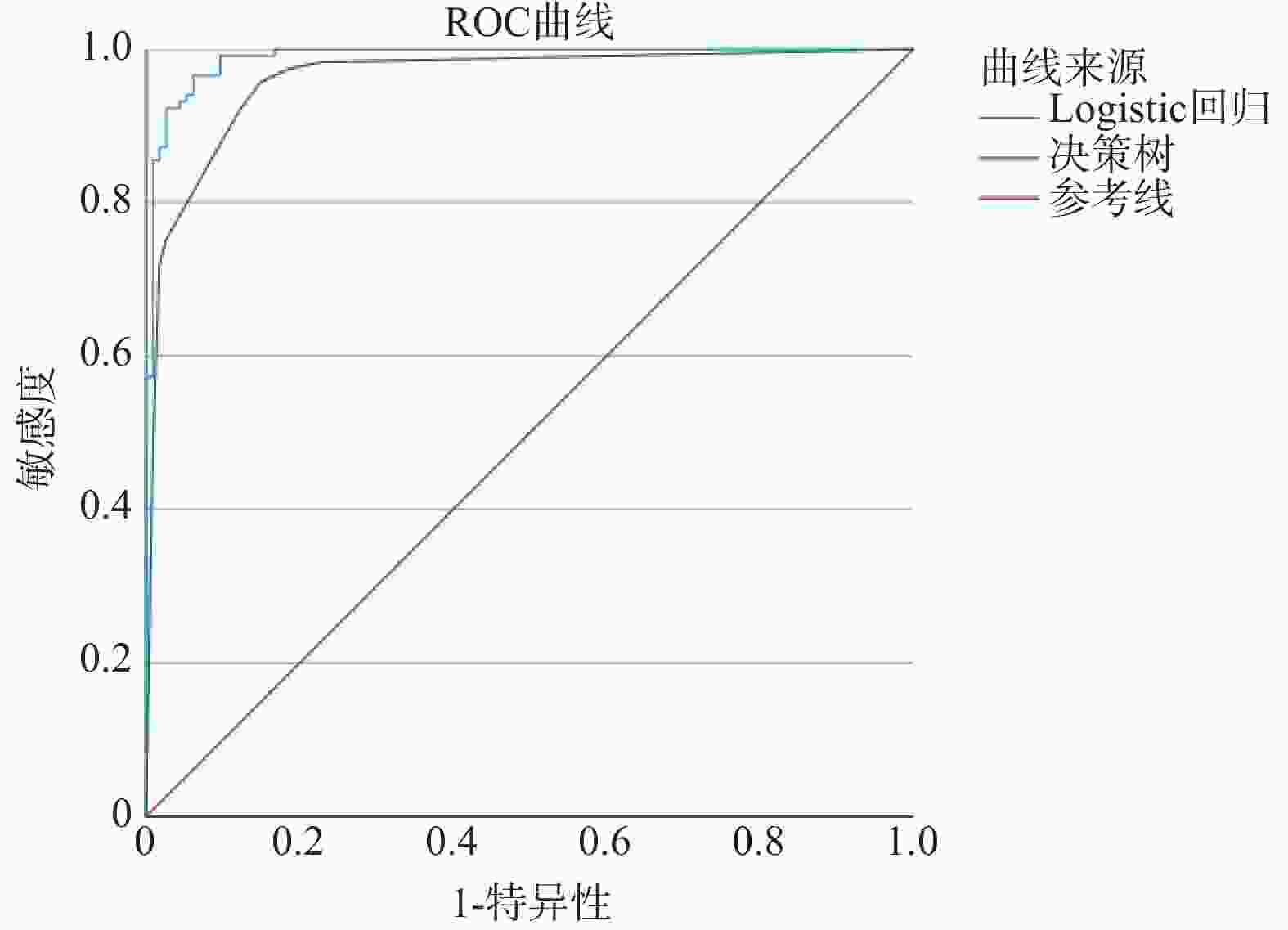
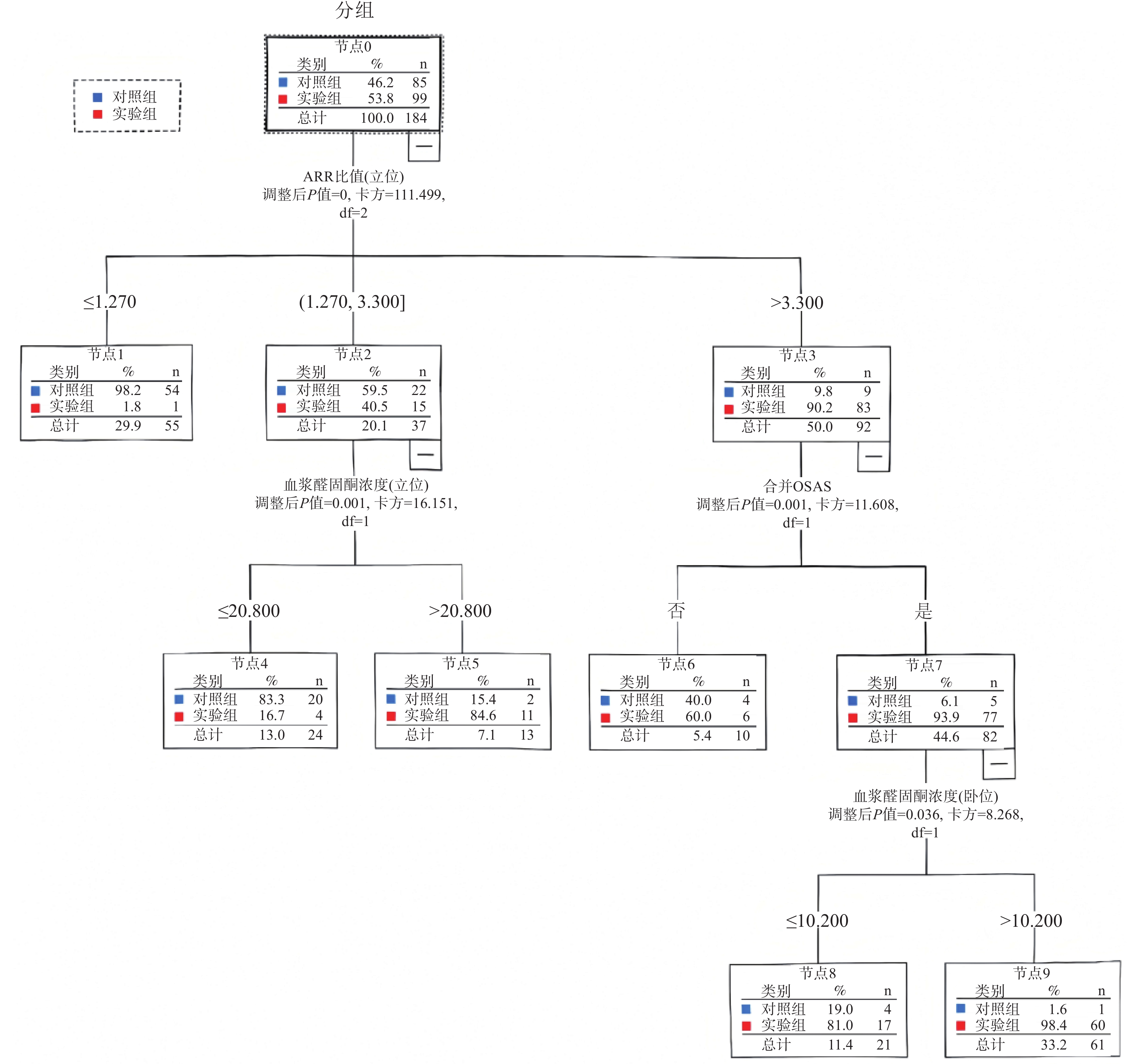
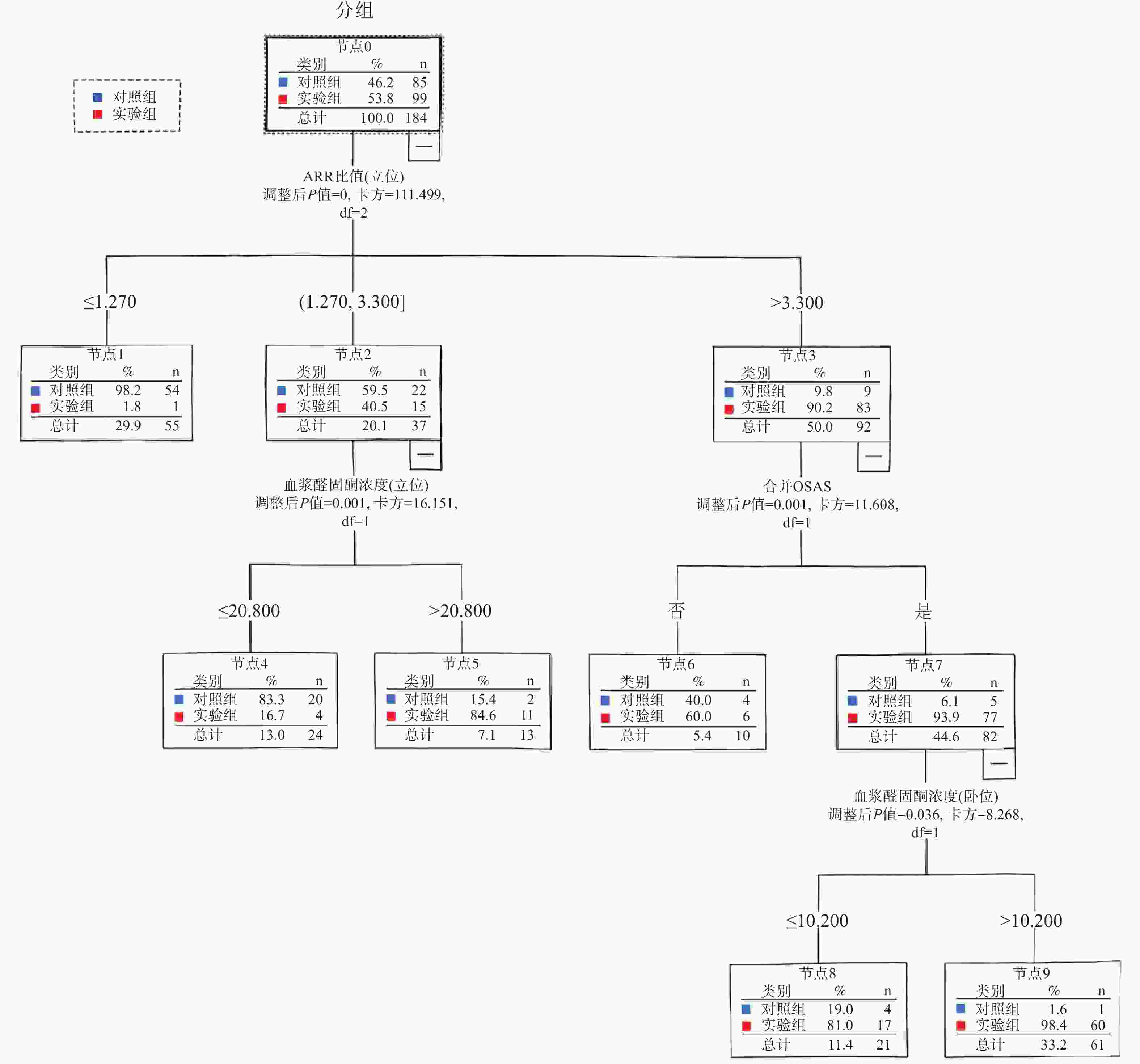
目的 采用Logistic回归与决策树模型预测高血压人群原发性醛固酮增多症(primary aldosteronism,PA)的危险因素。 方法 实验组为2024年1月至11月期间在云南省阜外心血管病医院确诊为PA的患者118例,对照组为同期经过继发性高血压筛查后确诊为原发性高血压的患者113例,建立Logistic回归与决策树预测模型,用受试者工作特征(receiver operating characteristic,ROC)曲线评价两种模型的预测效果。 结果 Logistic回归预测模型为:Logit(P) = 2.162×合并阻塞性睡眠呼吸暂停低通气综合征(obstructive sleep apnea hypopnea syndrome,OSAHS) − 0.145×年龄−2.140×血钾+0.429×血浆醛固酮浓度(卧位)−1.591×直接肾素浓度(卧位)+0.435× 血浆醛固酮浓度(立位)−0.150× 直接肾素浓度(立位);决策树分析筛选出4个风险变量,与PA相关的因素依次为醛固酮/肾素比值(aldosterone to renin concentration ratio,ARR)(立位)(P < 0.001)、血浆醛固酮浓度(立位)(P = 0.001)、合并OSAHS(P = 0.001)、血浆醛固酮浓度(卧位)(P = 0.036)。 结论 结合Logistic 回归和决策树模型预测,合并OSAHS、血浆醛固酮浓度(立位)、血浆醛固酮浓度(卧位)均可列为PA的独立危险因素;年龄、血钾、直接肾素浓度(卧位)、直接肾素浓度(立位)为保护因素。对于合并OSAHS、血浆醛固酮浓度(卧位) > 10.200 ng/dL的人群,可将 ARR切入点设置为3.300 ngdL−1/uIUmL−1,以降低临床PA的漏诊率。 -
关键词:
- 原发性醛固酮增多症 /
- 危险因素 /
- Logistic回归 /
- 决策树模型
Abstract:Objective To predict risk factors for primary aldosteronism (PA) in a hypertensive population using Logistic regression and decision tree models. Methods A case group of 118 patients diagnosed with PA and a control group of 113 patients diagnosed with essential hypertension after secondary hypertension screening were enrolled from the Fuwai Cardiovascular Hospital of Yunnan Province between January and November 2024. Logistic regression and decision tree prediction models were established, and the predictive performance of the two models was evaluated using the receiver operating characteristic(ROC)curve. Result The Logistic regression prediction model was: Logit(P) = 2.162 × (comorbid obstructive sleep apnea hypopnea syndrome, OSAHS) − 0.145 × age − 2.140 × serum potassium + 0.429 × plasma aldosterone concentration (recumbent) − 1.591 × direct renin concentration (recumbent) + 0.435 × plasma aldosterone concentration (upright) − 0.150 × direct renin concentration (upright). Decision tree analysis screened out four risk variables. Factors associated with PA, in order of importance, were: aldosterone-to-renin concentration ratio(ARR)(upright)(P < 0.001), plasma aldosterone concentration (upright)(P = 0.001), comorbid OSAHS(P = 0.001), and plasma aldosterone concentration (recumbent)(P = 0.036). Conclusion Based on the predictions from both the Logistic regression and decision tree models, comorbid OSAHS, plasma aldosterone concentration (upright), and plasma aldosterone concentration (recumbent) can be identified as independent risk factors for PA; while age, serum potassium, direct renin concentration (recumbent), and direct renin concentration (upright))are protective factors. For individuals with comorbid OSAHS and a plasma aldosterone concentration (recumbent) > 10.200 ng/dL, setting the ARR cut-off point at 3.300 ngdL−1/uIUmL−1 may help reduce the clinical missed diagnosis rate of PA. -
Key words:
- Primary aldosteronism /
- Risk factors /
- Logistic regression /
- Decision tree model
-
表 1 实验组与对照组单因素分析结果[n(%)/M(P25,P75)](1)
Table 1. Univariate analysis results of the case group and control groups [n(%)/M(P25,P75)](1)
变量 实验组(n = 118) 对照组(n = 113) χ2/Z P 性别 男 41(34.7) 73(64.6) 20.585 < 0.001* 女 77(65.3) 40(35.4) 年龄(岁) 49.5(43,55.25) 49(40,57) 0.042 0.837 BMI(kg/m2) 25.6(23.4,27.6) 25.9(23.8,28.7) 1.021 0.312 高血压病史(年) 4.00(1.00,9.00) 4.00(1.00,6.00) 0.469 0.494 脉压差(mmHg) 46(38.75,54) 46(35.5,54.5) 0.110 0.740 确诊前服用降压药物数量 2(0,3) 2(0,2) 4.302 0.038* 血钾(mmol/L) 3.82(3.49,4.11) 4.07(3.89,4.19) 23.336 < 0.001* 血钠(mmol/L) 139.50(138.25,141.13) 139.7(137.80,141.00) 0.523 0.470 白蛋白(g/L) 43.05(40.25,45.03) 42.60(40.70,45.30) 0.047 0.829 L-LDL(mmol/L) 3.04(2.56,3.60) 3.18(2.46,3.91) 0.548 0.459 HDL-C(mmol/L) 1.24(1.08,1.43) 1.15(1.02,1.36) 6.240 0.012* 血浆醛固酮(卧位)(ng/dL) 14.25(10.40,19.40) 9.41(5.85,12.85) 44.779 < 0.001* 血浆肾素浓度(卧位)(µIU/mL) 0.78(0.50,1.47) 7.74(2.66,16.51) 91.939 < 0.001* ARR比值(卧位)(ng·dL−1/µIU·mL−1) 17.89(7.82,25.95) 1.03(0.54,2.61) 126.545 < 0.001* 血浆醛固酮(立位)(ng/dL) 22.55(15.40,27.40) 13.10(8.38,18.40) 53.916 < 0.001* 血浆肾素浓度(立位)(µIU/mL) 2.72(1.02,5.32) 15.60(6.05,31.24) 73.081 < 0.001* 表 1 实验组与对照组单因素分析结果[n(%)/M(P25,P75)](2)
Table 1. Univariate analysis results of the case group and control groups [n(%)/M(P25,P75)](2)
变量 实验组(n = 118) 对照组(n = 113) χ2/Z P ARR比值(立位)(ng·dL−1/µIU·mL−1) 8.85(4.21,18.45) 0.91(0.45,1.58) 120.720 < 0.001* 吸烟史 有 27(22.9) 56(49.6) 17.843 < 0.001* 无 91(77.1) 57(50.4) 饮酒史 有 28(23.7) 45(39.8) 6.917 0.009* 无 90(76.3) 68(60.2) 高血压家族史 有 70(59.3) 65(57.5) 0.077 0.781 无 48(40.7) 48(42.5) 高血压分级 2 11(9.3) 13(11.5) 0.295 0.587 3 107(90.7) 100(88.5) 肾动脉狭窄 是 5(4.2) 2(1.8) 1.196 0.274 否 113(95.8) 111(98.2) 合并糖尿病 是 17(14.4) 14(12.4) 0.202 0.653 否 101(85.6) 99(87.6) 合并冠心病 是 39(33.1) 40(35.4) 0.141 0.707 否 79(66.9) 73(64.6) 合并甲状腺疾病 是 13(11.0) 13(11.5) 0.014 0.907 否 105(89.0) 100(88.5) 合并OSAHS 是 106(89.8) 63(55.8) 34.139 < 0.001* 否 12(10.2) 50(44.2) 合并高尿酸血症 是 50(42.4) 60(53.1) 2.662 0.103 否 68(57.6) 53(46.9) 肾上腺异常 是 45(38.1) 9(8.0) 29.335 < 0.001* 否 73(61.9) 104(92.0) 肝肾功能不全 是 12(10.2) 9(8.0) 0.340 0.560 否 106(89.8) 104(92.0) 尿蛋白 是 45(38.1) 42(37.2) 0.023 0.879 否 73(61.9) 71(62.8) *P < 0.05。 表 2 变量赋值
Table 2. Variable assignment
自变量 赋值方式 性别 女 = 0,男 = 1 年龄 实测值(岁) 血钾 实测值(mmol/L) 血钠 实测值(mmol/L) HDL-C 实测值(mmol/L) 血浆醛固酮浓度(卧位) 实测值(ng/dL) 血浆肾素浓度(卧位) 实测值(µIU/mL) ARR(卧位) 实测值(ng·dL−1/µIU·mL−1) 血浆醛固酮浓度(立位) 实测值(ng/dL) 血浆肾素浓度(立位) 实测值(µIU/mL) ARR(立位) 实测值(ng·dL−1/µIU·mL−1) 合并OSAHS 否 = 0,是 = 1 吸烟史 否 = 0,是 = 1 饮酒史 否 = 0,是 = 1 肾上腺异常 否 = 0,是 = 1 肝肾功能不全 否 = 0,是 = 1 表 3 多因素Logistic回归分析
Table 3. Multivariate Logistic regression analysis
变量 β SE Wald χ2 P OR 95%CI 性别 −1.613 1.290 1.563 0.211 0.199 0.016~2.498 年龄 −0.145 0.049 8.738 0.003* 0.865 0.785~0.952 血钾 −2.140 1.026 4.353 0.037* 0.118 0.016~0.878 血钠 −0.023 0.047 0.244 0.622 0.977 0.891~1.072 HDL-C 3.399 1.923 3.125 0.077 29.929 0.691~ 1296.130 血浆醛固酮浓度(卧位) 0.429 0.187 5.257 0.022* 1.536 1.064~2.217 血浆肾素浓度(卧位) −1.591 0.440 13.086 < 0.001* 0.204 0.086~0.482 ARR比值(卧位) −0.118 0.089 1.750 0.186 0.889 0.746~1.058 血浆醛固酮浓度(立位) 0.435 0.106 16.792 < 0.001* 1.545 1.255~1.901 血浆肾素浓度(立位) −0.150 0.071 4.502 0.034* 0.861 0.750~0.989 ARR比值(立位) −0.060 0.065 0.849 0.357 0.942 0.829~1.070 吸烟史 −1.651 1.191 1.921 0.166 0.192 0.019~1.981 饮酒史 0.941 1.081 0.758 0.384 2.563 0.308~21.338 合并OSAHS 2.162 0.895 5.834 0.016* 8.690 1.503~50.238 肾上腺异常 1.304 0.849 2.356 0.125 3.684 0.697~19.470 肝肾功能不全 0.358 1.076 0.111 0.739 1.431 0.174~11.794 常量 9.046 8.639 1.096 0.295 8480.673 *P < 0.05。 -
[1] Reincke M, Bancos I, Mulatero P, et al. Diagnosis and treatment of primary aldosteronism[J]. Lancet Diabetes Endocrinol, 2021, 9(12): 876-892. doi: 10.1016/S2213-8587(21)00210-2 [2] Brown J M, Siddiqui M, Calhoun D A, et al. The unrecognized prevalence of primary aldosteronism: A cross-sectional study[J]. Ann Intern Med, 2020, 173(1): 10-20. doi: 10.7326/M20-0065 [3] Douma S, Petidis K, Doumas M, et al. Prevalence of primary hyperaldosteronism in resistant hypertension: A retrospective observational study[J]. Lancet, 2008, 371(9628): 1921-1926. doi: 10.1016/S0140-6736(08)60834-X [4] Parasiliti-Caprino M, Lopez C, Prencipe N, et al. Prevalence of primary aldosteronism and association with cardiovascular complications in patients with resistant and refractory hypertension[J]. J Hypertens, 2020, 38(9): 1841-1848. doi: 10.1097/HJH.0000000000002441 [5] 蒋丹, 刘斌, 付凌云, 等. 环维黄杨星D对醛固酮诱导型心肌肥厚和凋亡的保护作用及机制[J]. 贵州医科大学学报, 2024, 49(2): 169-178. doi: 10.19367/j.cnki.2096-8388.2024.02.002 [6] Vaidya A, Mulatero P, Baudrand R, et al. The expanding spectrum of primary aldosteronism: Implications for diagnosis, pathogenesis, and treatment[J]. Endocr Rev, 2018, 39(6): 1057-1088. [7] Xu Z, Yang J, Hu J, et al. Primary aldosteronism in patients in China with recently detected hypertension[J]. J Am Coll Cardiol, 2020, 75(16): 1913-1922. doi: 10.1016/j.jacc.2020.02.052 [8] Funder J W, Carey R M, Mantero F, et al. The management of primary aldosteronism: Case detection, diagnosis, and treatment: An endocrine society clinical practice guideline[J]. J Clin Endocrinol Metab, 2016, 101(5): 1889-1916. [9] Song Y, Yang S, He W, et al. Confirmatory tests for the diagnosis of primary aldosteronism: A prospective diagnostic accuracy study[J]. Hypertension, 2018, 71(1): 118-124. doi: 10.1161/HYPERTENSIONAHA.117.10197 [10] Jain A, Baracco R, Kapur G. Pheochromocytoma and paraganglioma-an update on diagnosis, evaluation, and management[J]. Pediatr Nephrol, 2020, 35(4): 581-594. [11] 孟旭. 原发性醛固酮增多症临床特点、预后与心血管疾病危险因素研究[D]. 北京: 北京协和医学院, 2021. [12] Feng Y, Wang J, Shao Z, et al. Predicting related factors of immunological response to hepatitis B vaccine in hemodialysis patients based on integration of decision tree classification and logistic regression[J]. Hum Vaccin Immunother, 2021, 17(9): 3214-3220. doi: 10.1080/21645515.2021.1895603 [13] 刘幸, 李畏娴, 张乐, 等. 基于决策树和logistic回归构建恙虫病合并脓毒症的预测模型[J]. 中国热带医学, 2024, 24(9): 1066-1073. doi: 10.13604/j.cnki.46-1064/r.2024.09.08 [14] Arnaud C, Bochaton T, Pépin J L, et al. Obstructive sleep apnoea and cardiovascular consequences: Pathophysiological mechanisms[J]. Arch Cardiovasc Dis, 2020, 113(5): 350-358. doi: 10.1016/j.acvd.2020.01.003 [15] 张茹, 赵雅静, 张雯, 等. 高血压患者体力活动时长, 睡眠质量及体重控制对患者报告结局的影响[J]. 昆明医科大学学报, 2025, 46(2): 80-87. doi: 10.12259/j.issn.2095-610X.S20250212 [16] 马若菡, 田茗源, 王波. 原发性醛固酮增多症与阻塞性睡眠呼吸暂停低通气综合征关系的研究进展[J]. 中华高血压杂志, 2022, 30(12): 1147-1151. doi: 10.16439/j.issn.1673-7245.2022.12.012 [17] Zennaro M C, Boulkroun S, Fernandes-Rosa F L. Pathogenesis and treatment of primary aldosteronism[J]. Nat Rev Endocrinol, 2020, 16(10): 578-589. doi: 10.1038/s41574-020-0382-4 [18] Burrello J, Monticone S, Losano I, et al. Prevalence of hypokalemia and primary aldosteronism in 5100 patients referred to a tertiary hypertension unit[J]. Hypertension, 2020, 75(4): 1025-1033. doi: 10.1161/HYPERTENSIONAHA.119.14063 [19] Xu F, Gao Z, Wang G, et al. Prevalence, subtype classification, and outcomes of treatment of primary aldosteronism: A prospective study in China[J]. Endocr Pract, 2021, 27(5): 478-483. [20] Younes N, St-Jean M, Desrochers M J, et al. Usefulness of the upright posture test in the diagnosis of primary aldosteronism[J]. J Endocr Soc, 2024, 8(10): bvae155. doi: 10.1210/jendso/bvae155 [21] 中华医学会内分泌学分会. 原发性醛固酮增多症诊断治疗的专家共识(2020版)[J]. 中华内分泌代谢杂志, 2020, 36(9): 727-736. doi: 10.3760/cma.j.cn311282-20241115-00546 [22] 任亚女, 查晓宇, 董作亮. 醛固酮与直接肾素浓度比值筛查天津市高血压人群中原发性醛固酮增多症的最佳切点[J]. 中国慢性病预防与控制, 2024, 32(11): 827-831. doi: 10.16386/j.cjpccd.issn.1004-6194.2024.11.005 -





 下载:
下载: