Cultivating Critical Thinking Ability in Clinical Medical Students of Tumor Interventional Radiology through Case-Based Heuristic Teaching Method
-
摘要:
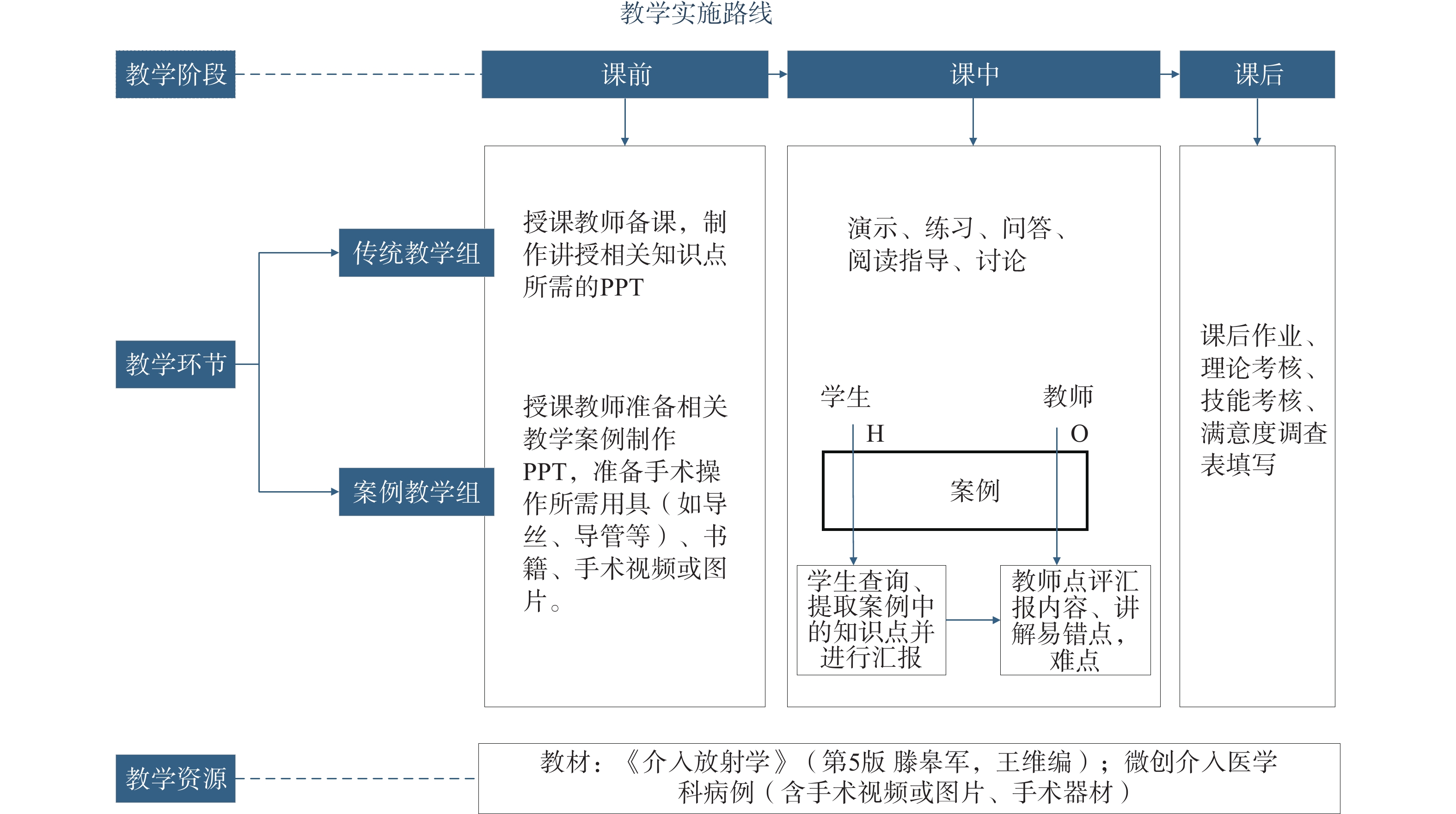
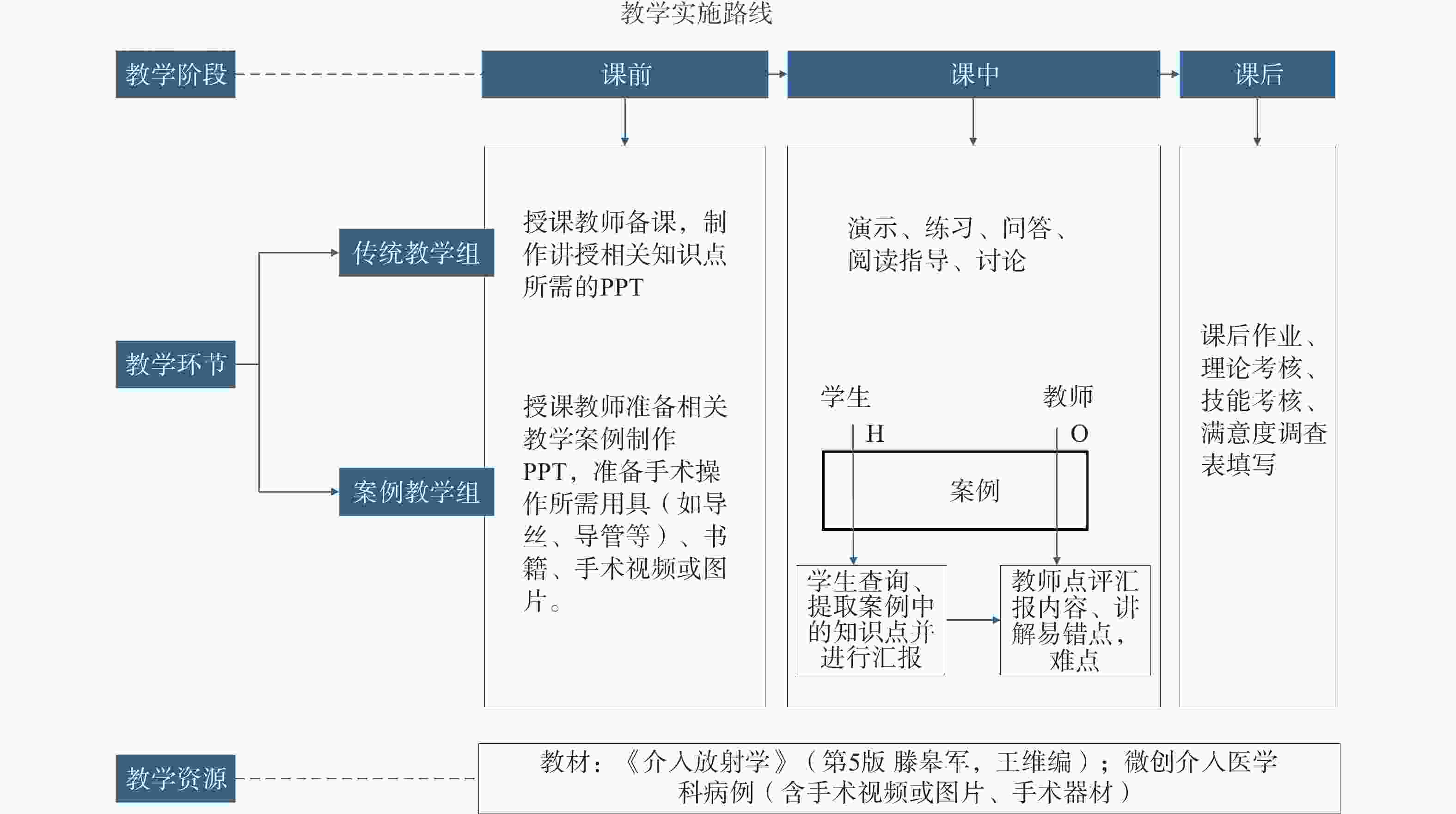
目的 探讨案例启发式教学法在培养肿瘤介入临床医学生批判性思维能力的应用价值。 方法 选择2023年6月至2024年12月由微创介入医学科授课《介入放射学》的本科学生120名作为研究对象,根据交替分组法分为传统教学组(n = 60,接受传统教学法授课)和案例教学组(n = 60,接受案例启发式教学法授课)。比较两组学生批判性思维能力测量表(CTDI-CV)得分,评估两组学生对临床带教的满意度,比较两组学生的综合考试结果和课程考核通过率。 结果 案例教学组综合考核平均得分为84.43分,传统教学组为81.93分;案例教学组和传统教学组学生课程考核通过率分别为98.33%(59/60)和93.33%(56/60)。两组综合得分与课程通过率比较,差异无统计学意义(P﹥0.05)。案例教学组学生教学后寻找真相、开放思想、分析能力、系统化能力、评判自信心、求知欲、认知成熟度及总评分高于传统教学组(P < 0.05);案例教学组学生课程满意度平均得分(14.22分)高于传统教学组(13.52分)(P < 0.05)。 结论 案例启发式教学法应用于培养肿瘤介入临床医学生的教学中能够有效提高学生的批判性思维能力,在不降低基础教学成效的前提下,能有效提高学生批判性思维能力与课程满意度,具有较高的推广应用价值。 Abstract:Objective To explore the application value of case-based heuristic teaching method in cultivating critical thinking ability among undergraduate medical students in tumor interventional radiology. A total of 120 undergraduate students enrolled in the course "Interventional Radiology" taught by the Department of Minimally Invasive Interventional Medicine from June 2023 to December 2024 were selected as research subjects. They were divided into two groups using alternating grouping method: traditional teaching group (n = 60, receiving conventional teaching method) and case-based teaching group (n = 60, receiving case-based heuristic teaching method). Critical thinking disposition inventory (CTDI-CV) scores were compared between the two groups, satisfaction with clinical teaching was assessed, and comprehensive examination results and course pass rates were compared. Results The average comprehensive assessment score for the case-based teaching group was 84.43 points, compared to 81.93 points for the traditional teaching group. The course pass rates for students in the case-based teaching group and traditional teaching group were 98.33% (59/60) and 93.33% (56/60), respectively. No statistically significant differences were found between the two groups in comprehensive scores and course pass rates (P > 0.05). After instruction, students in the case-based teaching group demonstrated significantly higher scores in truth-seeking, open-mindedness, analytical ability, systematicity, evaluative confidence, inquisitiveness, cognitive maturity, and overall critical thinking scores compared to the traditional teaching group (P < 0.05). The average course satisfaction score for the case-based teaching group (14.22 points) was significantly higher than that of the traditional teaching group (13.52 points) (P < 0.05). Conclusion The application of case-based heuristic teaching method in the instruction of undergraduate medical students in tumor interventional radiology can effectively enhance students' critical thinking ability. While maintaining the effectiveness of foundational teaching, this method can effectively improve students' critical thinking ability and course satisfaction, demonstrating high value for promotion and application. -
表 1 两组学生的综合考核得分比较 [分,($\bar x \pm s $)]
Table 1. Comparison of comprehensive assessment scores between the two groups [points,($\bar x \pm s $)]
组别 综合考核得分 t P 案例教学组 84.43 ± 7.058 1.535 0.128 传统教学组 81.93 ± 10.460 表 2 两组学生的课程通过率比较 [n(%)]
Table 2. Comparison of course pass rates between the two groups [n(%)]
组别 n 课程通过情况 χ2 P 通过 不通过 案例教学组 60 59(98.33) 1(1.7) 0.835 0.171 传统教学组 60 56(93.33) 4(6.7) 表 3 两组学生对课程满意度的比较 [分,M(P25,P75)]
Table 3. Comparison of course satisfaction between the two groups[points,M(P25,P75)]
类别 案例教学组 传统教学组 Z P 课程结构逻辑性 3(3~3) 3(2~3) −2.533 0.011* 内容与临床需求匹配度 3(3~3) 3(3~3) −0.525 0.600 介入技术的前沿性覆盖 3(3~3) 3(2~3) −3.146 0.002* 理论知识与实践结合度 3(3~3) 3(3~3) −0.151 0.880 课程难以适应性 3(3~3) 3(2~3) −1.700 0.089 总满意度得分 15(14~15) 14(13~14.75) −3.469 <0.001* *P < 0.05。 表 4 两组学生的CTDI-CV评分比较 (分,$\bar x \pm s $)
Table 4. Comparison of CTDI-CV scores between the two groups(points,$\bar x \pm s $)
维度 组别 案例教学组 传统教学组 t P 寻找真相 教学前 42.27 ± 6.984 41.58 ± 6.193 0.567 0.572 教学后 45.53 ± 5.809 42.28 ± 6.217 2.959 0.004* t −2.836 −1.562 P 0.006* 0.124 开放思想 教学前 41.43 ± 8.171 40.73 ± 7.539 0.488 0.627 教学后 45.23 ± 5.391 41.67 ± 7.808 2.912 0.004* t −2.917 −3.729 P 0.005* <0.001* 分析能力 教学前 40.87 ± 6.182 40.70 ± 5.9475 0.150 0.881 教学后 43.72 ± 5.009 40.53 ± 5.601 3.282 0.001* t −2.804 0.588 P 0.007* 0.559 系统化能力 教学前 40.42 ± 5.276 40.85 ± 5.132 −0.456 0.649 教学后 45.15 ± 5.004 40.80 ± 4.293 5.110 <0.001* t −4.564 0.114 P <0.001* 0.910 评判自信 教学前 41.93 ± 6.470 41.50 ± 6.275 0.372 0.710 教学后 44.65 ± 5.960 41.43 ± 6.099 2.922 0.004* t −2.373 0.000 P 0.021* 1.000 求知欲 教学前 41.92 ± 4.989 41.75 ± 4835 0.186 0.853 教学后 43.35 ± 4.554 42.82 ± 4.257 3.148 0.002* t −3.848 −3.642 P <0.01* <0.001* 认知成熟度 教学前 41.38 ± 5.811 41.43 ± 5.604 −0.048 0.962 教学后 44.45 ± 4.156 41.97 ± 5.666 2.738 0.007* t −3.107 −3.098 P 0.003* 0.03* 总评分 教学前 290.22 ± 32.170 288.55 ± 29.920 0.294 0.769 教学后 314.08 ± 25.186 291.50 ± 27.334 4.706 <0.001* t −4.257 −2.769 P <0.001* 0.008* *P < 0.05。 -
[1] 羽思, 李玥, 李骥, 等. 翻转课堂结合基于案例的协作学习在新型临床医学八年制教学中的应用[J]. 协和医学杂志, 2022, 13(1): 74-78. [2] 李建华, 张力燕, 杜晓华, 等. 循证医学PICOS模式结合导学式教学法与传统教学法在临床教学中的对照研究[J]. 昆明医科大学学报, 2014, 35(9): 165-167. doi: 10.3969/j.issn.1003-4706.2014.09.045 [3] 李艳英, 黄天生, 李雪微, 等. 浅析几种常见的医学教学方法[J]. 创新教育研究, 2022, 10(6): 1340-1344. doi: 10.12677/CES.2022.106216 [4] 安天志, 王黎洲, 周石. 介入放射学研究生教学的现状和问题分析[J]. 中国继续医学教育, 2015, 7(7): 13-14. doi: 10.3969/j.issn.1674-9308.2015.07.009 [5] 余结根, 陶香香, 刘影, 等. “考研热”影响下医学生临床实习中存在的问题和对策[J]. 卫生职业教育, 2015, 33(17): 95-97. [6] Cantillon P. Teaching large groups[J]. Bmj, 2003, 326(7386): 437. doi: 10.1136/bmj.326.7386.437 [7] 陈宏泉, 陆晓鸥, 江水, 等. 皮肤性病学临床教学CBL与LBL应用效果的Meta分析[J]. 青岛大学学报(医学版), 2020, 56(2): 241-244. [8] 陈彦蓓, 姚萍, 潘小丽, 等. PBL结合情景模拟在GTCS护理应急培训中的构建与应用[J]. 昆明医科大学学报, 2024, 45(11): 181-185. [9] Thistlethwaite J E, Davies D, Ekeocha S, et al. The effectiveness of case-based learning in health professional education. A BEME systematic review: BEME Guide No. 23[J]. Med Teach, 2012, 34(6): e421-e444. doi: 10.3109/0142159X.2012.680939 [10] 彭美慈, 汪国成, 陈基乐, 等. 批判性思维能力测量表的信效度测试研究[J]. 中华护理杂志, 2004, 39(9): 644-647. [11] Hussey I, Alsalti T, Bosco F, et al. An aberrant abundance of cronbach’s alpha values at. 70[J]. Adv Meth Pract Psychol Sci, 2025, 8: 25152459241287123. [12] 俞璐. 住院医师规范化培训中批判性思维能力的培养[J]. 中国病案, 2020, 21(11): 79-81. doi: 10.16659/j.cnki.1672-5654.2024.07.216 [13] Wang Y, Feng J. Effectiveness of participatory teaching methods in the standardized training of respiratory medicine residents[J]. J Contemp Educ Res, 2023, 7(10): 179-184. doi: 10.26689/jcer.v7i10.5494 [14] 杜翔宇, 楚尧娟, 乔高星. 药学生批判性思维能力现状调查与影响因素分析[J]. 中国药业, 2021, 30(14): 26-29. [15] 谢晓宇, 赵文霞. 世界一流大学本科生批判性思维培养研究——以斯坦福大学为例[J]. 外国教育研究, 2024, 51(10): 75-85. [16] 王文亮. 基于雨课堂的混合教学模式在介入放射学本科教学中的应用[J]. 中国继续医学教育, 2024, 16(11): 123-127. doi: 10.3969/j.issn.1674-9308.2024.11.026 [17] 魏宁, 徐浩, 祖茂衡, 等. 现阶段介入放射学临床实习影响因素探讨[J]. 2014, (9): 822-825. [18] 蒋天鹏, 王黎洲, 李兴, 等. 介入放射学本科生教学改革探讨[J]. 中国实用医药, 2014, 9(31): 272-273. doi: 10.14163/j.cnki.11-5547/r.2014.31.441 [19] 宋杰, 王黎洲, 周石. 基于深化介入放射学教学改革的介入放射学发展分析[J]. 中国继续医学教育, 2014, 6(3): 96-98. doi: 10.3969/J.ISSN.1674-9308.2014.03.062 [20] 吴思英, 杨华, 郑馥荔, 等. 公共卫生专业硕士教育教学案例库建设的思考与探索[J]. 沈阳医学院学报, 2022, 24(3): 320-324. doi: 10.16753/j.cnki.1008-2344.2022.03.023 [21] 郭亚春, 苏萌, 周晓慧, 等. 案例法教学在医学微生物学课程中的应用[J]. 2017, (13): 2023-2024. [22] 姚海欣, 王惠, 赵丽华. 案例启发式教学法在提升护理学院学生批判性思维能力的应用价值[J]. 中国高等医学教育, 2023(1): 116-117. [23] Dodd M A, Rafi J, Jakeman B, et al. A case-based learning exercise to increase students' understanding of the pharmacist’s role in public health interventions for individual patients[J]. Curr Pharm Teach Learn, 2020, 12(7): 817-826. doi: 10.1016/j.cptl.2020.02.004 [24] 马俊花, 顾明君, 孙菲, 等. 启发式结合案例教学法在内分泌科的临床教学作用[J]. 继续医学教育, 2020, 34(7): 23-25. doi: 10.3969/j.issn.1004-6763.2020.07.013 [25] 于健, 刘晓玲, 柳玮明. 启发式临床医学教学法结合案例教学法在内分泌科临床教学中的应用价值[J]. 医学理论与实践, 2019, 32(11): 1791-1793. doi: 10.16659/j.cnki.1672-5654.2021.24.024 [26] 阮华玲, 杨坤, 杜亮, 等. 启发式临床医学与案例教学法在内分泌科临床教学中的应用[J]. 中国继续医学教育, 2024, 16(11): 63-67. [27] 王春燕, 曹靖玮, 王菲, 等. 培养医学生批判性思维的教学模式初探[J]. 中国继续医学教育, 2023, 15(10): 37-41. [28] Ma C, Zhou W. Effects of unfolding case-based learning on academic achievement, critical thinking, and self-confidence in undergraduate nursing students learning health assessment skills [EB/OL]. Nurse Education in Practice, 2022, 60: 103321. (2022-03-08) [2025-12-16]. https://pubmed.ncbi.nlm.nih.gov/35287002/. [29] Shafique A, Ur Rehman A, Ibnerasa S, et al. Case-based learning in undergraduate orthodontic education: A cross sectional study[EB/OL]. (2024-11-05) [2025-12-02]. https://pmc.ncbi.nlm.nih.gov/articles/PMC11380727/. [30] Alizadeh M, Saramad A, Rafiepoor H, et al. Effect of virtual case-based learning (CBL) using the flipped class and peer instruction on the motivation to learn basic sciences[J]. BMC Med Educ, 2024, 24(1): 1230. doi: 10.1186/s12909-024-06229-w [31] 黄学卿, 江哲宇, 许敏, 等. 模拟教学在介入放射学微课程教学改革中的应用[J]. 中华介入放射学电子杂志, 2022, 10(3): 316-319. doi: 10.3877/cma.j.issn.2095-5782.2022.03.017 [32] Ghatan C E, Kuo W T, Hofmann L V, et al. Making the case for early medical student education in interventional radiology: A survey of 2nd-year students in a single U. S. institution[J]. J Vasc Interv Radiol, 2010, 21(4): 549-553. doi: 10.1016/j.jvir.2009.12.397 [33] 张文广, 曾军杰, 任建庄, 等. 基于问题学习教学法联合基于案例学习教学法在肿瘤介入放射学临床教学中的应用[J]. 2025, (3): 426-428. [34] Abosalem Y. Assessment techniques and students’higher-order thinking skills[J]. Int J Second Educ, 2016, 4(1): 1. [35] 南华大学衡阳医学院. 四种教学法简介[EB/OL]. (2014-09-22)[2025-12-18]. https://yxy.usc.edu.cn/info/2131/1218.htm. [36] Taber K S. The use of cronbach’s alpha when developing and reporting research instruments in science education[J]. Res Sci Educ, 2018, 48(6): 1273-1296. doi: 10.1007/s11165-016-9602-2 [37] Bujang M A, Omar E D, Baharum N A. A review on sample size determination for cronbach’s alpha test: A simple guide for researchers[J]. Malays J Med Sci, 2018, 25(6): 85-99. doi: 10.21315/mjms2018.25.6.9 [38] Tavakol M, Dennick R. Making sense of cronbach’s alpha[J]. Int J Med Educ, 2011, 2: 53-55. -





 下载:
下载: