An Epidemiological Analysis of 1500 Pediatric Burns Patients at the Burn Center in Yunnan
-
摘要:
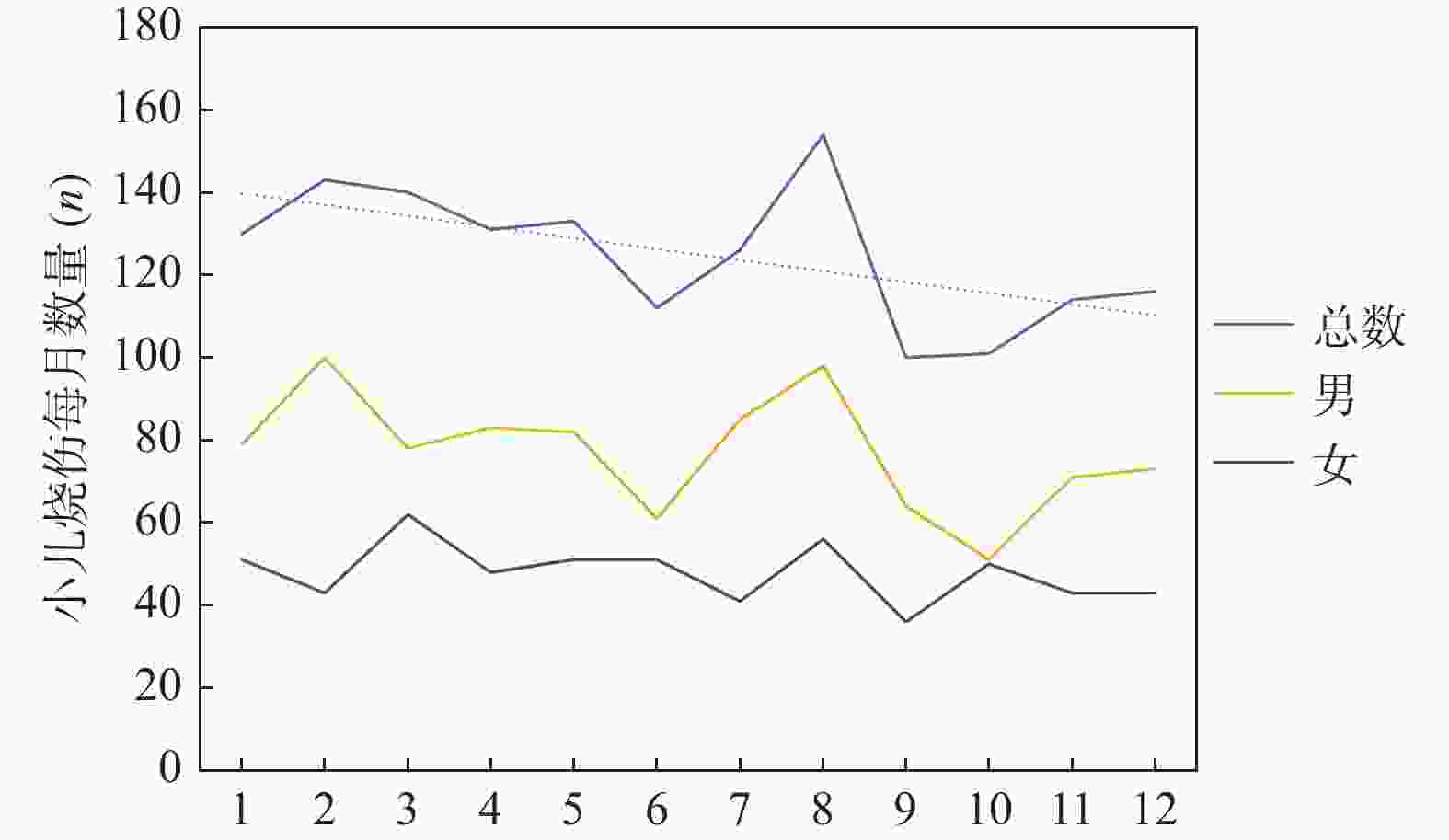
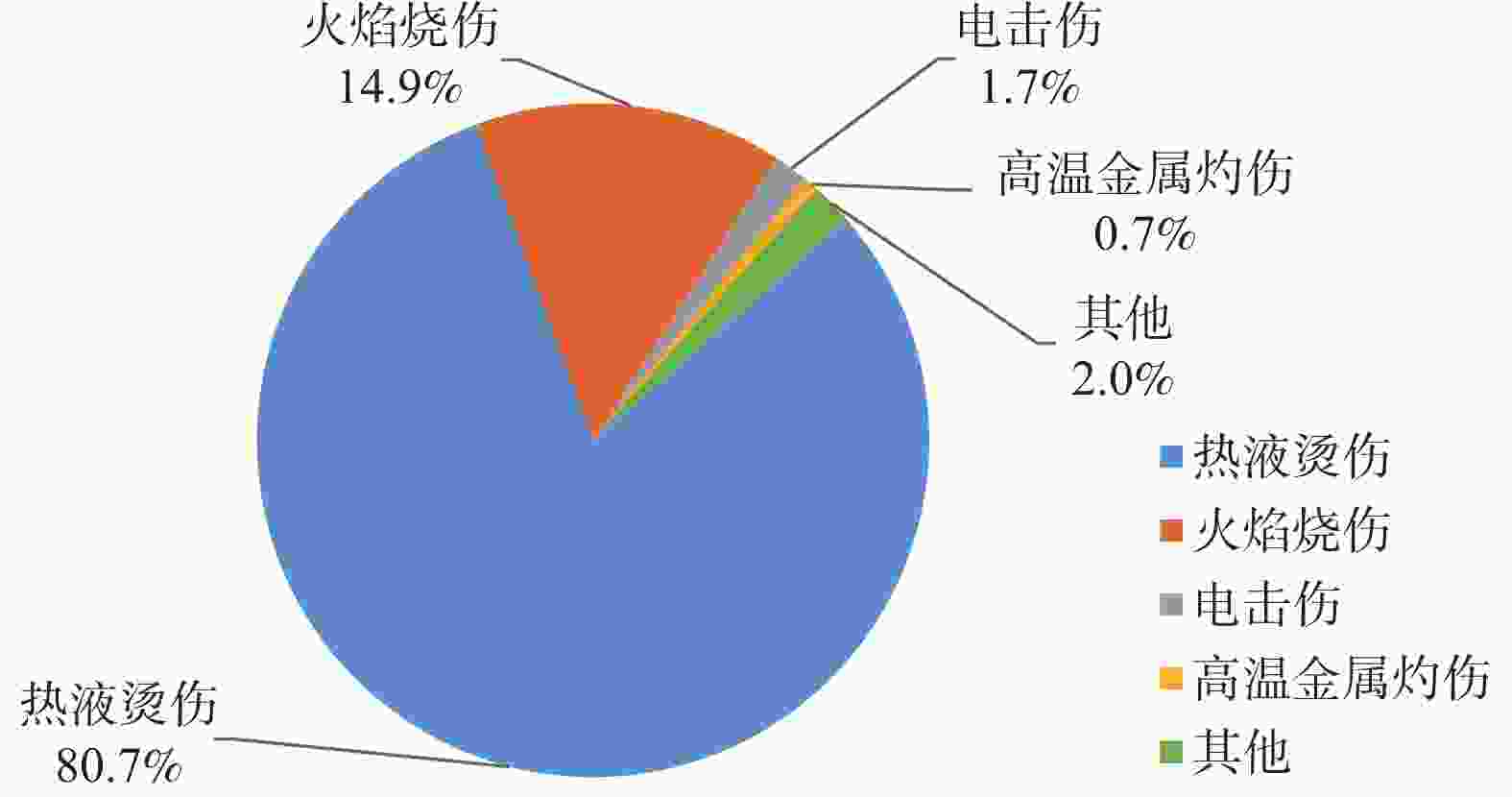
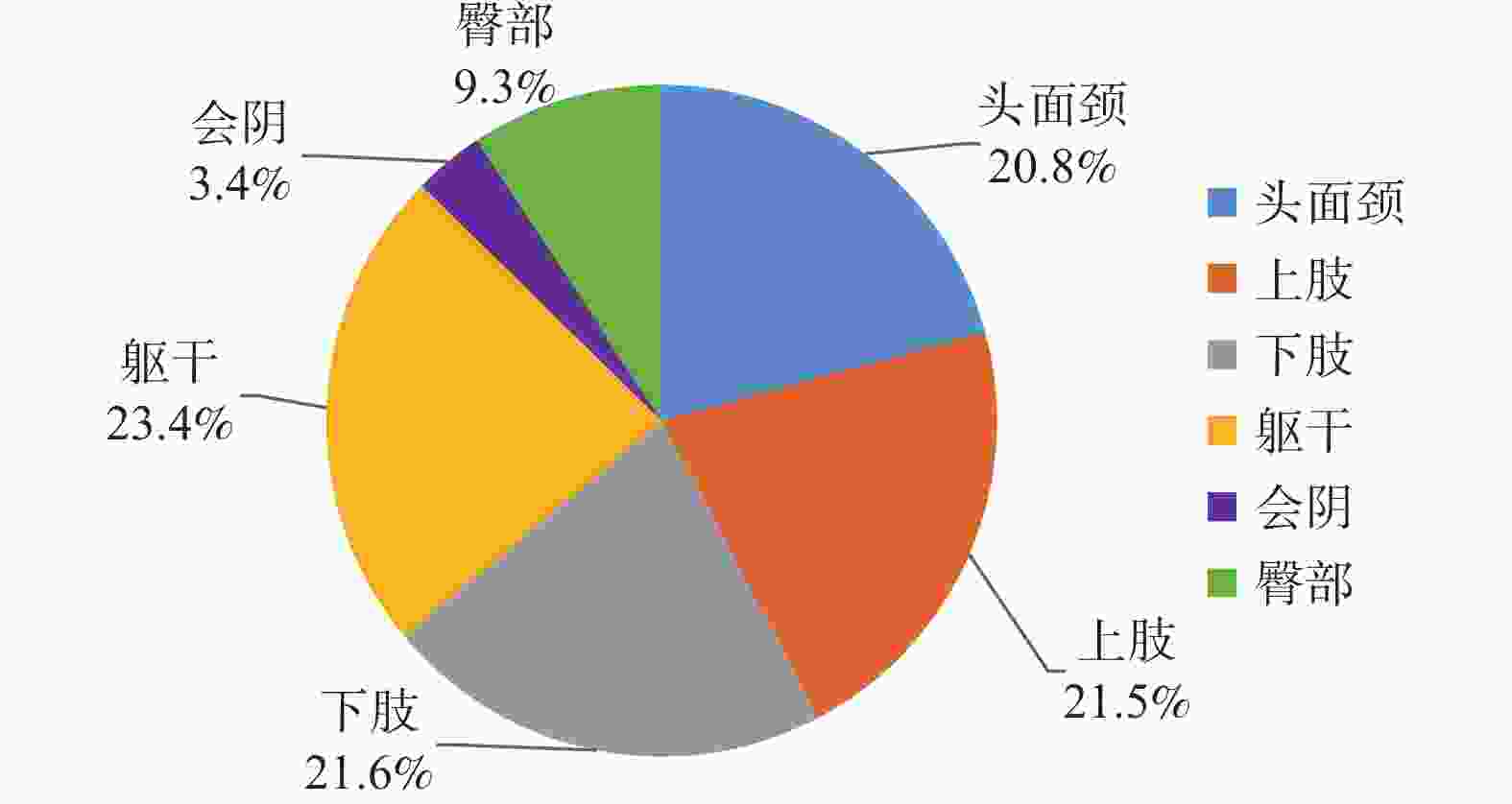
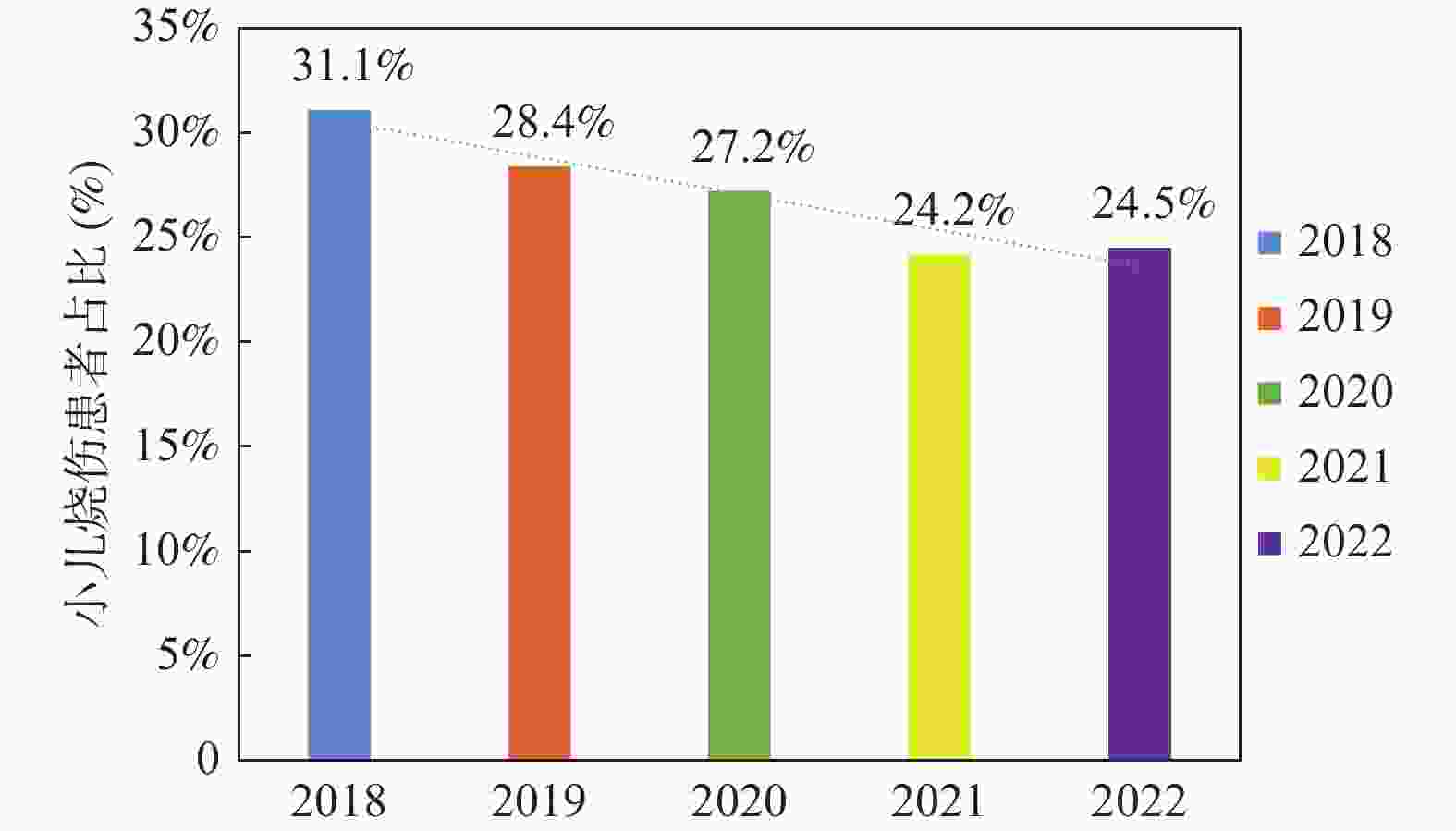
目的 研究云南省小儿烧伤流行病学的特点。 方法 收集2018年1月1日至2022年12月31日收治于昆明医科大学第二附属医院烧伤科的 1500 例小儿烧伤患者的住院资料,对小儿烧伤患者的年龄、性别、烧伤发生时间、烧伤类型、烧伤面积、烧伤部位、小儿烧伤患者同期占比、住院时长、付费方式、住院费用、居住地等特点进行统计分析。结果 小儿烧伤最容易发生时期为幼儿期(873例,58.2%),男性儿童相较于女性儿童更易发生烧伤(男∶女=1.9∶1);最常发季节为春季(n = 404,26.9%);热液烫伤为主要致伤类型(n = 1211 ,81.0%);小儿烧伤严重程度以中度烧伤为主(n = 945,63.0%);统计小儿烧伤最大面积为98.0% TBSA,最小面积为0.1% TBSA,烧伤平均面积$ \overline{x} $为14.5% TBSA,中值为10.0% TBSA;小儿烧伤最常发生部位为躯干(n = 982,23.4%);2018一2022年小儿烧伤患者占同期烧伤患者占比逐年下降(χ2 = 18.852,P < 0.001),小儿烧伤患者平均住院时长为12.4 d,平均住院费用为15667.08 元;小儿烧伤患者家庭居住地大部分位于县级及以下地区(n =1027 ,68.5%);烧伤危重程度、治疗方式、是否有并发症与小儿烧伤的临床结局有影响,差异均有统计学意义(χ2 = 23.453,P < 0.001)。结论 小儿烧伤患者呈现出一系列显著的特点。小儿烧伤患者以男性为主,好发年龄主要集中在幼儿期,春季被确定为最为多发的季节,而秋季则相对较少。热液烫伤是主要的烧伤类型,以中度烧伤为主,烧伤平均面积约为14.5% TBSA,四肢、躯干被确定为烧伤好发部位。近年居民对于小儿烧伤的预防意识逐渐提高,小儿烧伤患者占比存在明显的下降趋势。 Abstract:Objective To study the characteristics of pediatric burn epidemiology in this area. Methods Data of 1500 pediatric burn patients admitted to the Burn Department of the Second Affiliated Hospital of Kunming Medical University from January 1, 2018 to December 31, 2022 were collected. The age, sex, time of burn occurrence, type of burn, burn area, burn site, proportion of pediatric burn patients in the same period, length of hospitalization, payment method, hospitalization cost and residence of pediatric burn patients were statistically analyzed.Results The most common time for childhood burns to occur is during early childhood (873 cases, 58.2%), with male children more likely to suffer burns compared to female children (male∶female = 1.9∶1). The most frequent season for these burns is spring (404 cases, 26.9%). Scalding from hot liquids is the primary cause of injury ( 1211 cases, 81.0%). Most childhood burns are classified as moderate severity (945 cases, 63.0%). The maximum burn area recorded was 98.0% TBSA, the minimum was 0.1% TBSA, the average burn area was 14.5% TBSA, and the median was 10.0% TBSA. The most common site of burns in children is the trunk (982 cases, 23.4%). From 2018 to 2022, the proportion of pediatric burn patients among all burn patients has been decreasing annually (χ2 = 18.852, P < 0.001). The average length of hospitalization for pediatric burn patients was 12.4 days, with an average hospitalization cost of15667.08 yuan. Most of the families of pediatric burn patients live in county-level areas or below (1027 cases, 68.5%). The severity of the burns, treatment methods, and presence of complications all significantly affect the clinical outcomes of pediatric burns, with statistically significant differences (χ2 = 23.453, P < 0.001).Conclusion Pediatric burn patients exhibit a range of significant characteristics. The majority of these patients are male, with the most common age group being toddlers. Spring has been identified as the season with the highest incidence of burns, while autumn sees relatively fewer cases. Scald injuries from hot liquids are the most common type of burn, with moderate burns being the most prevalent. The average burn area is approximately 14.5% of the total body surface area (TBSA). The limbs and trunk are the most commonly affected areas. In recent years, there has been a noticeable decrease in the proportion of pediatric burn patients, which is attributed to the growing awareness of burn prevention among the general population. -
Key words:
- Burns /
- Child /
- Clinical data analysis /
- Therapy /
- Prevention
-
表 1 小儿烧伤严重程度分类标准[1]
Table 1. Classification criteria for severity of pediatric burns
严重程度 表现 轻度 I 度和 II 度烧伤总面积< 5% 。 中度 烧伤总面积5% ~ 15%或III度烧伤面积<5%。 重度 烧伤总面积16% ~ 25%III度烧伤面积为 5% ~ 10% 。
另有下列情形之一者,虽然烧伤总面积< 15%,也视为重度;
①伴有眼烧伤、面颈部烧伤、手烧伤、会阴部烧伤或吸入性烧伤者;
②全身情况严重,有并发症或休克者;
③有严重创伤或合并化学药物中毒者;
④婴儿头面部烧伤面积>5% 者。特重度 烧伤总面积>25%或III度烧伤面积>10%。 表 2 小儿烧伤年龄段分布
Table 2. Distribution of age groups in pediatric burns
时期 n 占比(%) 新生儿期+婴儿期 82 5.5 幼儿期 873 58.2 学龄前期 336 22.4 学龄期 209 13.9 合计 1500 100.0 表 3 小儿烧伤季节分布与性别分布[n(%)]
Table 3. Seasonal and gender distribution of pediatric burns [n(%)]
季节 性别(n) 数值 男 女 春季 243 161 404(26.9) 夏季 244 127 392(26.1) 秋季 186 129 315(21.0) 冬季 252 137 389(25.9) 合计 925 554 1500 (100.0)χ2 5.11 P 0.164 表 5 小儿烧伤患者的临床结局与单种因素是否有关联的分析[n(%)]
Table 5. Analysis of the clinical outcomes of pediatric burn patients and their association with single factors[n(%)]
因素 计数资料 总数 临床结局(n) χ2 P 理想 不理想 烧伤危重程度 轻度 168(11.2) 157 11 23.453 <0.001* 中度 945(63.0) 931 14 重度 146(9.7) 140 6 特重度 241(16.1) 226 15 治疗方式 手术、换药 376(25.1) 371 5 4.532 0.033* 仅换药 1124 (74.9)1085 39 是否自费 自费 345(23.0) 329 16 3.720 0.054 非自费 1155 (77.0)1125 30 并发症 有 344(22.9) 323 21 6.490 0.011* 无 1156 (77.1)1120 36 *P < 0.05。 表 4 小儿烧伤患者居住地点分布以及性别分布[n(%)]
Table 4. Distribution of residence and gender among pediatric burn patients[n(%)]
居住地 总数 性别(n) 男 女 县级及以下 1027 (68.5)629 398 县级以上 473(31.5) 295 178 χ2 0.172 P 0.690 -
[1] 黎鳌. 黎鳌烧伤学[M]. 上海: 上海科学技术出版社,2001: 12. [2] Cuttle L,Fear M,Wood F M,et al. Management of non-severe burn wounds in children and adolescents: Optimising outcomes through all stages of the patient journey[J]. The Lancet Child & Adolescent Health,2022,6(4):269-278. [3] Peck M D. Epidemiology of burns throughout the world. Part I: Distribution and risk factors[J]. Burns,2011,37(7):1087-1100. [4] Chinese Burn Association. Expert consensus on the management of deep partial-thickness burn wounds in pediatric patients (2023 version)[J]. Zhonghua Shao Shang Yu Chuang Mian Xiu Fu Za Zhi,2023,39(10):901-910. [5] 李勇,许瑾,章祥洲,等. 1 552例小儿烧伤流行病学特点分析[J]. 中华损伤与修复杂志(电子版),2014,9(5):506-511. [6] 田俊英,李如兵,郭光华,等. 江西烧伤中心2 517例小儿烧伤患者流行病学分析[J]. 感染. 炎症. 修复,2018,19(4):232-236. [7] 香燕,闫芳,苏金虎,等. 河西某地区431例小儿烧伤病例分析及预防要点[J]. 中国妇幼健康研究,2021,32(4):495-498. [8] 蒋薇,胡德林,周舜英,等. 1737例小儿烧伤临床特点分析[J]. 安徽医学,2019,40(5):511-513. [9] 林国安. 小儿烧伤流行特点和早期处理[J]. 中华损伤与修复杂志(电子版),2018,13(4):247-252. [10] 魏冬. 甘肃省某医院儿童烧伤住院患者流行病学和临床特征分析[D]. 银川: 宁夏医科大学,2020. [11] Moser W J,Bilka K R,Vrouwe S Q,et al. Running water while bathing is a risk factor for pediatric scald burns[J]. Burns,2023,49(7):1714-1718. doi: 10.1016/j.burns.2023.03.014 [12] 赵倩,励晓红,严子淇,等. 中国5岁以下儿童2009—2019年意外伤害死亡趋势分析[J]. 中国儿童保健杂志,2023,31(10):1136-1141. [13] 付晋凤,张梦思. 儿童烧伤治疗及瘢痕防治策略的探讨[J]. 中华损伤与修复杂志(电子版),2018,13(4):241-246. [14] 周玉新,张林,陈明星,等. 湿润烧伤膏致小儿烧伤死亡11例分析[J]. 中华烧伤杂志,2003,19(5):34. [15] 岳长路,吴竹便,万萍,等. 外用湿润烧伤膏致肾功能衰竭和低温脓毒症死亡二例[J]. 中华烧伤杂志,2003,19(3):54. [16] Storey K,Kimble R M,Holbert M D. The management of burn pain in a pediatric burns-specialist hospital[J]. Pediatric Drugs,2021,23(1):1-10. doi: 10.1007/s40272-020-00434-y [17] Jeffs D,Dorman D,Brown S,et al. Effect of virtual reality on adolescent pain during burn wound care[J]. Journal of Burn Care & Research,2014,35(5):395-408. [18] Hill D M,DeBoer E. State and future science of opioids and potential of biased-ligand technology in the management of acute pain after burn injury[J]. Journal of Burn Care & Research,2023,44(3):524-534. [19] Hong N,Jung M H,Kim J W,et al. Opioid analgesics and depressive symptoms in burn patients: What is the real relationship?[J]. Clinical Psychopharmacology and Neuroscience,2016,14(3):295. [20] Khan A,Parikh M,Minhajuddin A,et al. Opioid prescribing practices in a pediatric burn tertiary care facility: Is it time to change?[J]. Burns,2020,46(1):219-224. [21] Farzan R,Parvizi A,Haddadi S,et al. Effects of non‐pharmacological interventions on pain intensity of children with burns: A systematic review and meta‐analysis[J]. International Wound Journal,2023,20(7):2898-2913. [22] Xiang H,Shen J,Wheeler K K,et al. Efficacy of smartphone active and passive virtual reality distraction vs standard care on burn pain among pediatric patients: A randomized clinical trial[J]. JAMA Network Open,2021,4(6):e2112082-e2112082. [23] Nischwitz S P,Luze H,Popp D,et al. Global burn care and the ideal burn dressing reloaded—A survey of global experts[J]. Burns,2021,47(7):1665-1674. [24] Chipp E,Charles L,Thomas C,et al. A prospective study of time to healing and hypertrophic scarring in paediatric burns: Every day counts[J]. Burns & Trauma,2017,5(3). https://doi.org/10.1186/s41038-016-0068-2 [25] Hall C,Hardin C,Corkins C J,et al. Pathophysiologic mechanisms and current treatments for cutaneous sequelae of burn wounds[J]. Comprehensive Physiology,2011,8(1):371-405. [26] Amini-Nik S,Yousuf Y,Jeschke M G. Scar management in burn injuries using drug delivery and molecular signaling: Current treatments and future directions[J]. Advanced Drug Delivery Reviews,2018,123:135-154. [27] Shpichka A,Butnaru D,Bezrukov E A,et al. Skin tissue regeneration for burn injury[J]. Stem cell Research & Therapy,2019,10:1-16. [28] Zhang Y,Niu X,Dong X,et al. Bioglass enhanced wound healing ability of urine‐derived stem cells through promoting paracrine effects between stem cells and recipient cells[J]. Journal of Tissue Engineering and Regenerative Medicine,2018,12(3):e1609-e1622. [29] Snider M D H,Young S,Enlow P T,et al. Coping in pediatric burn survivors and its relation to social functioning and self-concept[J]. Frontiers in Psychology,2021,12:695369. doi: 10.3389/fpsyg.2021.695369 [30] De Young A C,Kenardy J A,Cobham V E,et al. Prevalence,comorbidity and course of trauma reactions in young burn‐injured children[J]. Journal of Child Psychology and Psychiatry,2012,53(1):56-63. [31] Kazis L E,Lee A F,Rose M,et al. Recovery curves for pediatric burn survivors: advances in patient-oriented outcomes[J]. JAMA Pediatrics,2016,170(6):534-542. [32] 郭琳瑛,邱林,郑成中,等. 儿童烧伤预防和现场救治专家共识[J]. 中国当代儿科杂志,2021,23(12):1191-1199. -






 下载:
下载: