Clinical Study on Predicting Pregnancy Outcomes through the Imbalance of Vaginal Microbiota and Levels of Inflammatory Factors in Pregnant Women
-
摘要:
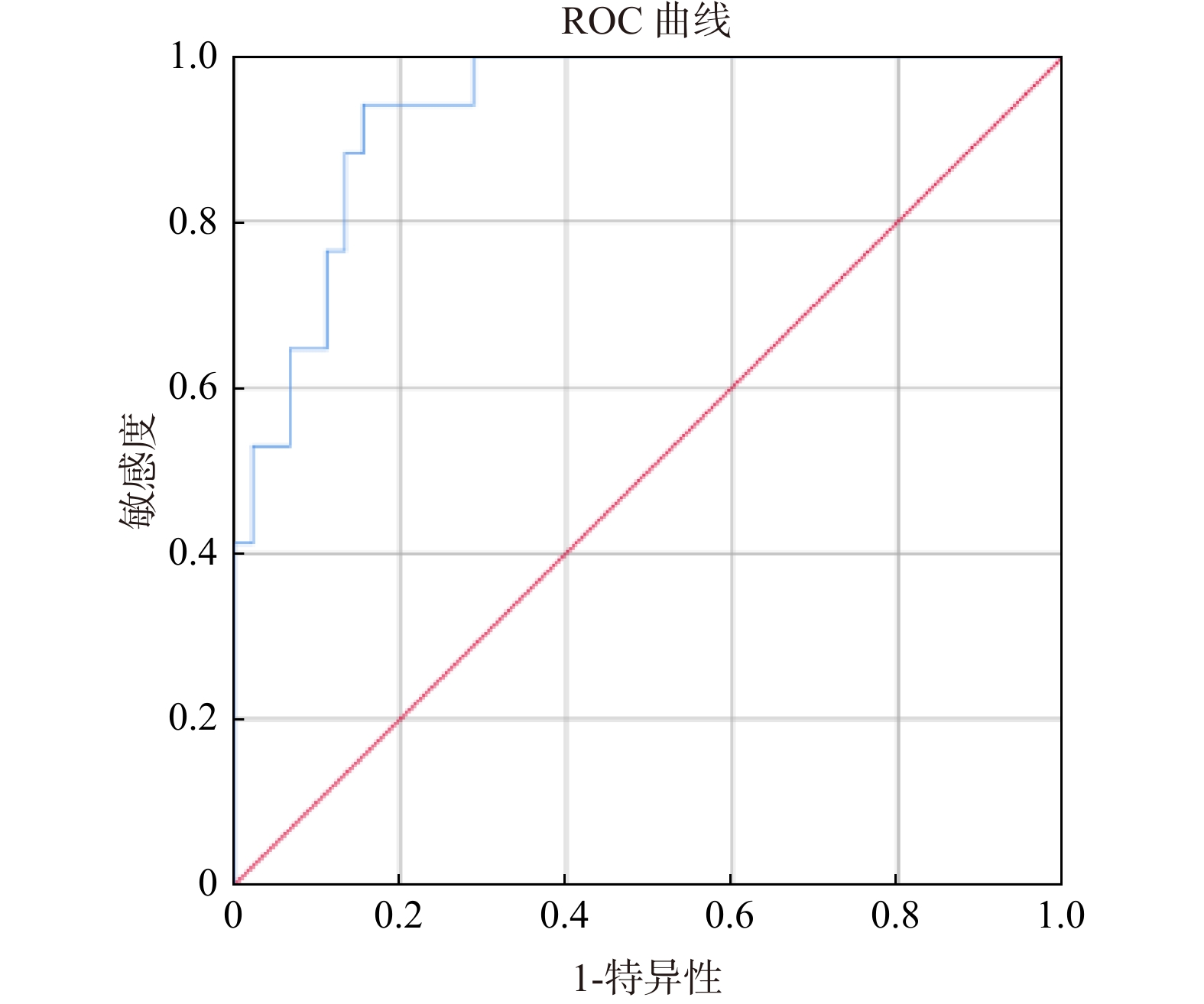
目的 探索孕妇阴道微生态异常与炎症因子水平对妊娠结局的预测价值。 方法 采用前瞻性队列分析衡水市妇幼保健院2022年12月至2023年12月妇产科接受孕检的400例妊娠晚期女性临床资料。采集产妇阴道分泌物,并接受阴道微生态检测,采用酶联免疫法检测高敏C反应蛋白(high-sensitivity C-reactive protein,hs-CRP)、降钙素原(procalcitonin,PCT)以及白细胞介素-6(interleukin-6,IL-6)水平。追踪阴道微生态检测结果及孕妇妊娠结局,根据阴道微生态结果分为观察组(微生态失衡,n = 200例)、对照组(微生态正常,n = 200例);根据妊娠结局分为良好组(n = 316例)、不良组(n = 84例)。对比观察组、对照组基线资料及不良妊娠结局;对比妊娠结局良好组、不良组临床特征;采用Logistic回归分析不良妊娠结局影响因素;采用受试者工作特征曲线(receiver operating characteristic curve analysis,ROC)分析阴道微生态与炎症因子水平对不良妊娠结局的预测效能。 结果 观察组hs-CRP、PCT、IL-6水平、不良妊娠结局(胎膜早破、早产、绒毛膜羊膜炎、新生儿感染)及总发生均高于对照组(P < 0.05)。妊娠结局不良组hs-CRP、PCT、IL-6水平、阴道菌群密集度I、IV、多样性I、IV、优势菌为非革兰阳性杆菌、念珠菌阳性、阴道pH≥4.5占比均高于良好组(P < 0.05)。Logistic回归分析显示,hs-CRP、PCT、IL-6水平、阴道菌群密集度及多样性I、IV级、优势菌为非革兰阳性杆菌、念珠菌阳性、阴道pH≥4.5均为不良妊娠结局危险因素(OR > 1,P < 0.05)。ROC曲线结果显示,预测价值曲线下面积(area under the curve,AUC)为0.914(0.856~0.937)。 结论 阴道微生态失衡与炎症因子构建预测不良妊娠结局价值较高。 Abstract:Objective To explore the impact of tracking the imbalance of vaginal microbiota in pregnant women and the level of inflammatory factors on predicting pregnancy outcomes. Method A prospective cohort study was conducted to analyze the clinical data of 400 late pregnancy women who underwent prenatal examinations in the obstetrics and gynecology department of Hengshui Maternal and Child Health Hospital from December 2022 to December 2023. Collect vaginal secretions from parturients and undergo vaginal microbiota testing. Use enzyme-linked immunosorbent assay to detect hs CRP, PCT, and IL-6 levels. Track the results of vaginal microbiota testing and pregnancy outcomes of pregnant women, and divide them into an observation group (imbalanced microbiota, n = 200) and a control group (normal microbiota, n = 200) based on the results of vaginal microbiota testing.According to pregnancy outcomes, they were divided into a good group (n = 316) and an adverse group (n = 84). Compare baseline data and adverse pregnancy outcomes between the vaginal microbiota imbalance group and the normal group. Compare the clinical characteristics of the group with good pregnancy outcomes and the group with poor pregnancy outcomes. Using logistic regression to analyze the influencing factors of adverse pregnancy outcomes. The predictive efficacy of ROC analysis on vaginal microbiota and inflammatory factor levels for adverse pregnancy outcomes. Results The levels of hs CRP, PCT, IL-6, adverse pregnancy outcomes (premature rupture of membranes, premature birth, chorioamnionitis, neonatal infection), and overall incidence rate in the group with vaginal microbiota imbalance were higher than those in the normal group (P < 0.05). The proportion of hs CRP, PCT, IL-6 levels, vaginal microbiota density I, IV, diversity I, IV, dominant bacteria being non Gram positive bacteria, Candida positive, and vaginal pH ≥ 4.5 in the group with poor pregnancy outcomes were higher than those in the normal group (P < 0.05). Logistic regression analysis showed that hs CRP, PCT, IL-6 levels, vaginal microbiota density and diversity levels I and IV, dominant bacteria being non Gram positive bacilli, Candida positive, and vaginal pH ≥ 4.5 were all risk factors for adverse pregnancy outcomes (OR > 1, P < 0.05). The ROC curve results show that the predictive value AUC (95%CI) is 0.914 (0.856~0.937). Conclusion Vaginal microecological imbalance and inflammatory factor construction have high value in predicting adverse pregnancy outcomes. -
Key words:
- Pregnancy period /
- Vaginal microbiota /
- Inflammatory factors /
- Pregnancy outcome /
- Influence factor
-
表 1 观察组与对照组基线资料及不良妊娠结局比较[n(%)/($\bar x \pm s $),n = 200]
Table 1. Comparison of baseline characteristics and adverse pregnancy outcomes between the observation and control groups[n(%)/($\bar x \pm s $),n = 200]
特征 观察组 对照组 χ2/t P 年龄(岁) 28.43 ± 3.49 28.56 ± 3.21 0.388 0.698 入组时孕周(周) 36.34 ± 1.26 36.17 ± 1.35 1.302 0.194 产次(次) 0.84 ± 0.12 0.86 ± 0.11 1.738 0.083 孕次(次) 1.59 ± 0.10 1.60 ± 0.07 1.159 0.247 体重指数(kg/m2) 23.31 ± 2.67 23.45 ± 2.06 0.587 0.558 hs-CRP(mg/L) 41.27 ± 2.35 8.65 ± 2.10 146.376 <0.001* PCT(pg/mL) 5.34 ± 0.67 0.97 ± 0.12 90.796 <0.001* IL-6(ng/L) 20.42 ± 5.67 3.11 ± 0.32 43.106 <0.001* 不良妊娠结局比较 67(33.50) 17(8.50) 37.673 <0.001* *P < 0.05。 表 2 妊娠结局良好组与不良组临床特征及炎症指标比较[n(%)/($\bar x \pm s $)]
Table 2. Comparison of clinical characteristics and inflammatory markers between groups with good and poor pregnancy outcomes[n(%)/($\bar x \pm s $)]
特征 良好组(n=316) 不良组(n=84) χ2/t P 年龄(岁) 28.17 ± 2.56 28.62 ± 2.43 1.447 0.149 入组时孕周(周) 36.10 ± 1.57 36.43 ± 1.25 1.782 0.076 产次(次) 0.83 ± 0.15 0.85 ± 0.14 1.101 0.272 孕次(次) 1.58 ± 0.23 1.60 ± 0.27 0.682 0.496 体重指数(kg/m2) 23.37 ± 2.11 23.50 ± 2.14 0.500 0.617 阴道菌群密集度 II~III 212(83.79) 41(16.21) 9.539 0.002* I、IV 104(70.75) 43(29.25) 多样性 II~III 249(84.12) 47(15.88) 18.001 <0.001* I、IV 67(64.42) 37(35.58) 优势菌 革兰阳性杆菌 279(82.54) 59(17.46) 16.513 <0.001* 其他 37(59.68) 25(40.32) 病原微生物 BV阳性 25(67.57) 12(32.43) 3.212 0.073 滴虫阳性 10(66.67) 5(33.33) 1.429 0.232 念珠菌阳性 34(64.15) 19(35.85) 8.120 0.004* 阴道pH ≥4.5 98(66.23) 50(33.77) 24.142 <0.001* <4.5 218(86.49) 34(13.51) hs-CRP(mg/L) 8.06 ± 1.28 40.37 ± 2.12 176.096 <0.001* PCT(pg/mL) 0.84 ± 0.11 5.27 ± 0.87 88.196 <0.001* IL-6(ng/L) 3.12 ± 0.35 20.15 ± 1.56 178.436 <0.001* *P < 0.05。 表 3 变量赋值表(含参考类别)
Table 3. Variable assignment table (including reference categories)
变量 赋值说明 参考类别 hs-CRP(mg/L) 连续变量,原值纳入 - PCT(pg/mL) 连续变量,原值纳入 - IL-6(ng/L) 连续变量,原值纳入 - 阴道菌群密集度 II-III=0,I/IV=1 II~III 多样性 II-III=0,I/IV=1 II~III 优势菌 革兰阳性杆菌=0,其他=1 革兰阳性杆菌 念珠菌感染 阴性=0,阳性=1 阴性 阴道pH值 <4.5=0,≥4.5=1 <4.5 产次(次) 连续变量,原值纳入 - BMI(kg/m2) 连续变量,原值纳入 - 表 4 Logistic回归分析不良妊娠结局的影响因素
Table 4. Logistic regression analysis of factors associated with adverse pregnancy outcomes
因素 β SE Waldχ2 P OR(95%CI) 阴道菌群密集度I、IV级 0.335 0.130 6.608 0.010* 1.398(1.083~1.805) 多样性I、IV级 0.340 0.145 5.525 0.019* 1.406(1.058~1.867) 优势菌为非革兰阳性杆菌 0.737 0.323 5.187 0.023* 2.089(1.108~3.937) 念珠菌阳性 0.705 0.316 5.032 0.025* 1.627(1.256~1.958) 阴道pH≥4.5 0.684 0.302 4.957 0.029* 1.567(1.258~1.786) hs-CRP 0.653 0.295 4.874 0.034* 1.532(1.244~1.723) PCT 0.258 0.134 10.276 0.002* 2.257(1.314~2.867) IL-6 0.326 0.135 5.432 0.018* 1.648(1.326~2.032) 常量 2.458 1.576 10.234 <0.001* *P < 0.05。 表 5 阴道微生态与炎症因子预测不良妊娠结局的ROC曲线分析
Table 5. ROC curve analysis of vaginal microecology and inflammatory factors for predicting adverse pregnancy outcomes
项目 最佳临界值 灵敏度(%) 特异度(%) AUC(95%CI) 预测价值 0.0534 93.45 87.23 0.914(0.856~0.937) -
[1] Yee L M, Miller E C, Greenland P. Mitigating the long-term health risks of adverse pregnancy outcomes[J]. JAMA, 2022, 327(5): 421-422. doi: 10.1001/jama.2021.23870 [2] Gleason J L, Grewal J, Chen Z, et al. Risk of adverse maternal outcomes in pregnant women with disabilities[J]. JAMA Netw Open, 2021, 4(12): e2138414-e2138414. doi: 10.1001/jamanetworkopen.2021.38414 [3] Barry V G, Johnson T N, Herrick C, et al. Adverse pregnancy outcomes and postpartum care as a pathway to future health[J]. Clin Obstet Gynecol, 2022, 65(3): 632-647. doi: 10.1097/GRF.0000000000000724 [4] Li X, Zhang Z, Bai H, et al. Analysis of vaginal microbiota during postpartum and postmenopausal periods based on metagenomics[J]. BMC Microbiol, 2024, 24(1): 501. [5] Lan J, Chen C. The role of lactic acid bacteria in maintaining vaginal internal environment homeostasis in patients with infertility[J]. Microb Pathog, 2023, 176: 106004. doi: 10.1016/j.micpath.2023.106004 [6] Gao Y, Shang Q, Wei J, et al. The correlation between vaginal microecological dysbiosis-related diseases and preterm birth: A review[J]. Med Microecol, 2021, 8: 100043. doi: 10.1016/j.medmic.2021.100043 [7] Gai S, Wu Q, Zhang H. The change of inflammatory status and vaginal flora in pregnant women with premature rupture of membranes[J]. J Med Microbiol, 2023, 72(4): 001678. [8] Shen L, Wang W, Hou W, et al. The function and mechanism of action of uterine microecology in pregnancy immunity and its complications[J]. Front Cell Infect Microbiol, 2023, 12: 1025714. doi: 10.3389/fcimb.2022.1025714 [9] Zhang W, Wan Y, Zhang Y, et al. Vaginal microecological imbalance and expression of serum inflammatory factors in pregnant women with group B streptococcus infection and pregnancy outcome[J]. Cell Mol Biol (Noisy-le-grand), 2023, 69(15): 148-153. doi: 10.14715/cmb/2023.69.15.26 [10] Nannan M, Xiaoping L, Ying J. Periodontal disease in pregnancy and adverse pregnancy outcomes: Progress in related mechanisms and management strategies[J]. Front Med (Lausanne), 2022, 9: 963956. doi: 10.3389/fmed.2022.963956 [11] Li S Q, Li F F. Effects of probiotic therapy combined with personalized nursing on immune function and nursing compliance in children with acute gastroenteritis[J]. Afr J Reprod Health, 2024, 28(11): 96-104. doi: 10.29063/ajrh2024/v28i11.10 [12] Dong X, Chen X, Xue M, et al. Changes in serum inflammatory factors in group B streptococcal infection and their predictive value for premature rupture of membranes complicated by chorioamnionitis[J]. Biomark Med, 2024, 18(7): 301-309. doi: 10.2217/bmm-2023-0588 [13] Afroz S. Comparison between the outcome of multiple and singleton pregnancy[J]. Insight, 2024, 7(2): 84-89. [14] Chen D, Gao X, Yang T, et al. Independent risk factors for placental abruption: A systematic review and meta-analysis[J]. BMC Pregnancy Childbirth, 2025, 25(1): 351. doi: 10.1186/s12884-025-07482-7 [15] Shen L, Zhang W, Yuan Y, et al. Vaginal microecological characteristics of women in different physiological and pathological period[J]. Front Cell Infect Microbiol, 2022, 12: 959793. doi: 10.3389/fcimb.2022.959793 [16] Deka N, Hassan S, Seghal Kiran G, et al. Insights into the role of vaginal microbiome in women's health[J]. J Basic Microbiol, 2021, 61(12): 1071-1084. doi: 10.1002/jobm.202100421 [17] Lee S, Oh K Y, Hong H, et al. Community state types of vaginal microbiota and four types of abnormal vaginal microbiota in pregnant korean women[J]. Front Public Health, 2020, 8: 507024. doi: 10.3389/fpubh.2020.507024 [18] 乔益梦, 范倩倩, 张小妹, 等. 妊娠期糖尿病阴道微生态与不良围产结局的研究进展[J]. 医学研究与战创伤救治, 2023, 36(7): 780-784. [19] 王丽, 于霞, 沈伟, 等. 妊娠晚期孕妇阴道微生态与B族溶血性链球菌感染的相关性分析[J]. 中国计划生育和妇产科, 2021, 13(8): 80-82. doi: 10.3969/j.issn.1674-4020.2021.08.21 [20] 张云霞, 吴东宁, 杜英, 等. 妊娠晚期孕妇阴道微生态失调与B族链球菌感染对母婴结局的影响[J]. 中国计划生育学杂志, 2020, 28(7): 1104-1107. [21] 郭海红, 王永凯, 郭丽丽. 妊娠期B族溶血性链球菌对孕妇凝血功能阴道微生态及妊娠结局的影响[J]. 河北医学, 2022, 28(8): 1375-1379. doi: 10.3969/j.issn.1006-6233.2022.08.030 [22] Romero R, Theis K R, Gomez-Lopez N, et al. The vaginal microbiota of pregnant women varies with gestational age, maternal age, and parity[J]. Microbiol Spectr, 2023, 11(4): e0342922. doi: 10.1128/spectrum.03429-22 [23] 崔微微, 吕玲玲, 王亚静, 等. 炎性因子、心功能指标与子痫前期孕妇妊娠结局的相关性分析[J]. 解放军医药杂志, 2022, 34(8): 59-63. doi: 10.3969/j.issn.2095-140X.2022.08.013 [24] Kara A E, Guney G, Tokmak A, et al. The role of inflammatory markers hs-CRP, sialic acid, and IL-6 in the pathogenesis of preeclampsia and intrauterine growth restriction[J]. Eur Cytokine Netw, 2019, 30(1): 29-33. [25] 姬建秀, 白惠, 王蕊. 孕晚期GBS定植或感染产妇血清PCT、IL-6、CCL-1水平与妊娠结局的关系[J]. 中国病案, 2022, 23(4): 102-105. doi: 10.3969/j.issn.1672-2566.2022.04.035 [26] 侯雪楠, 赵淑霞, 顾来梅. 妊娠晚期胎膜早破孕妇阴道菌群分布、微生态情况及与妊娠结局的关系[J]. 临床误诊误治, 2022, 35(5): 95-98. doi: 10.3969/j.issn.1002-3429.2022.05.029 [27] 谢萍, 肖燕, 罗汝琼, 等. B族链球菌孕妇感染血清炎症因子、Th1/Th2、β-hCG的变化及其对胎膜早破、妊娠结局的预测价值[J]. 中国现代医学杂志, 2021, 31(21): 78-85. doi: 10.3969/j.issn.1005-8982.2021.21.013 [28] 杨露, 孙晓红, 荆玉慧, 等. 妊娠晚期宫内感染B族链球菌对孕妇血清炎症因子的影响及妊娠结局分析[J]. 中国计划生育学杂志, 2022, 30(6): 1352-1356. [29] 林建丽, 凌奕, 陈华, 等. B族链球菌感染对孕妇阴道微生态失衡和血清炎性因子与母婴结局的影响[J]. 中华医院感染学杂志, 2022, 32(3): 462-465. [30] 杨仪心, 叶小凤, 劳力, 等. CRP、PCT、IL-6检测在妊娠晚期GBS感染患者妊娠结局预测中的价值[J]. 中国性科学, 2020, 29(1): 91-94. -





 下载:
下载: