Prevalence and Influence Factors of Renal Function Impairment in Patients Following Radical Cystectomy:A Systematic Review and Meta-analysis
-
摘要:
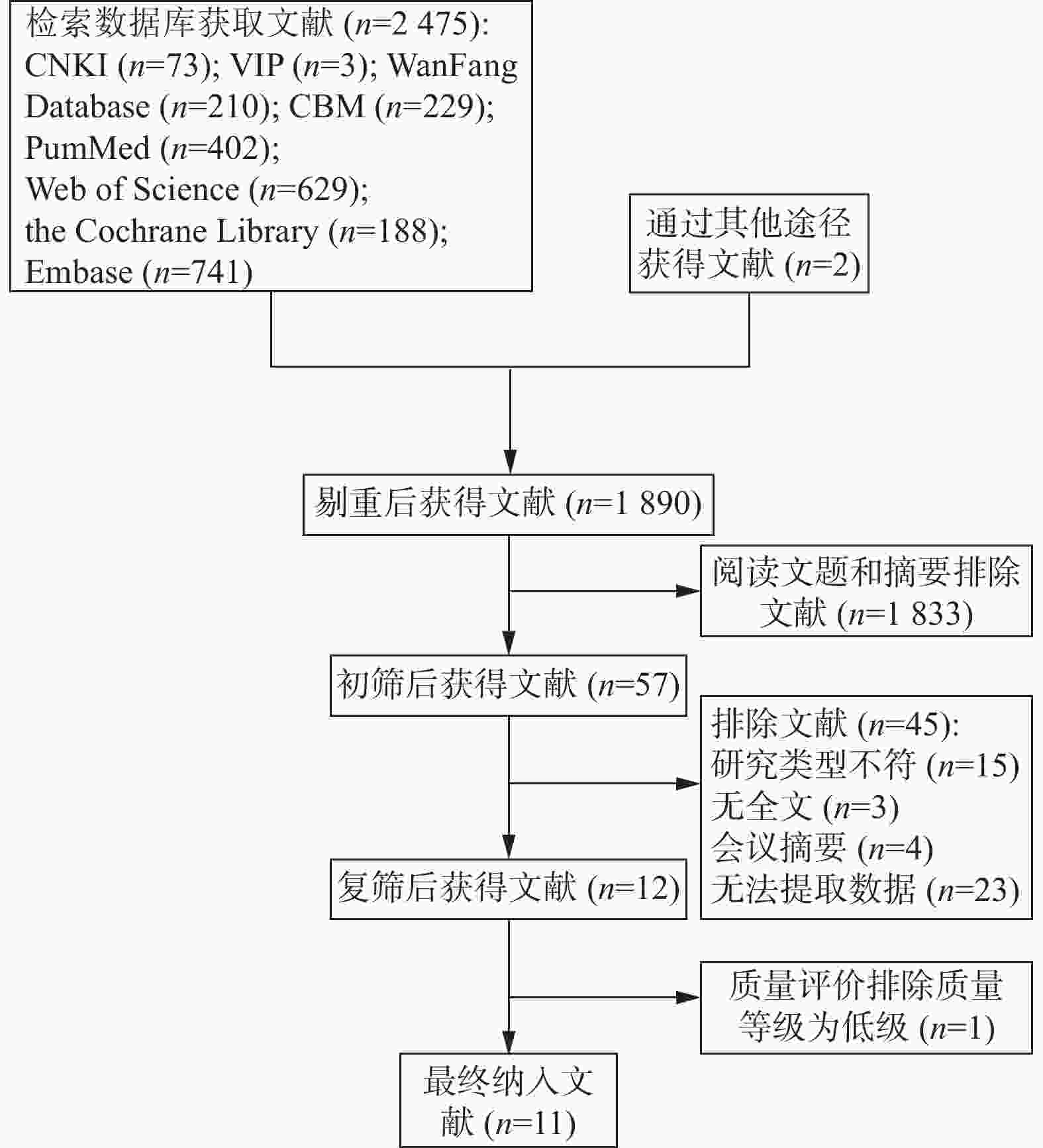
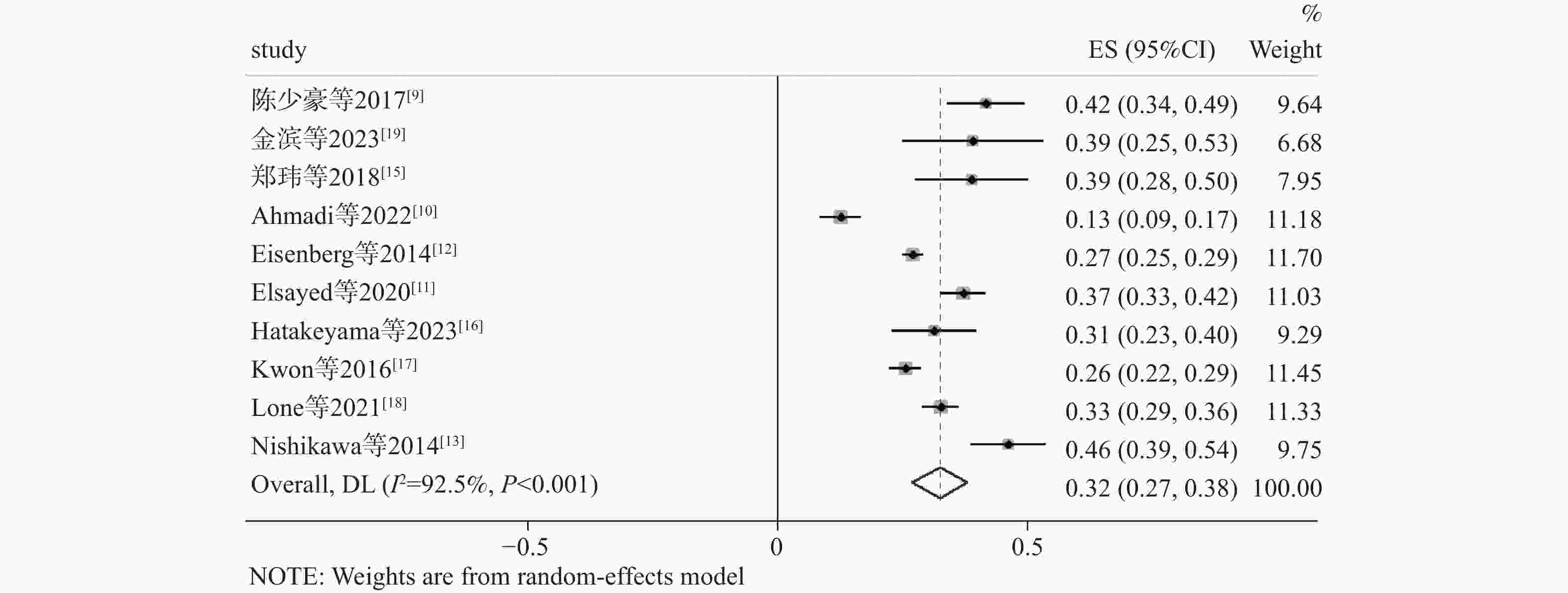
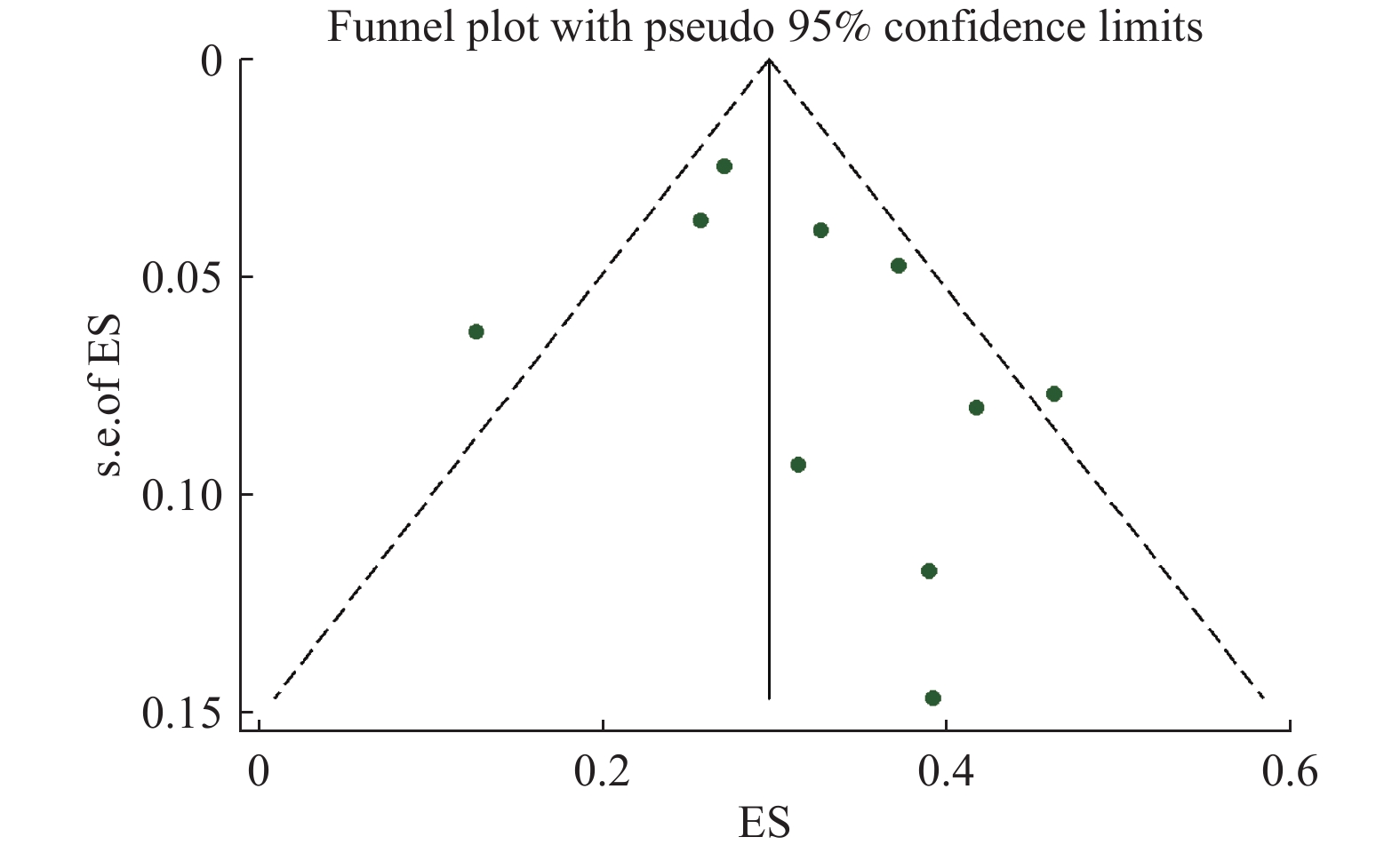
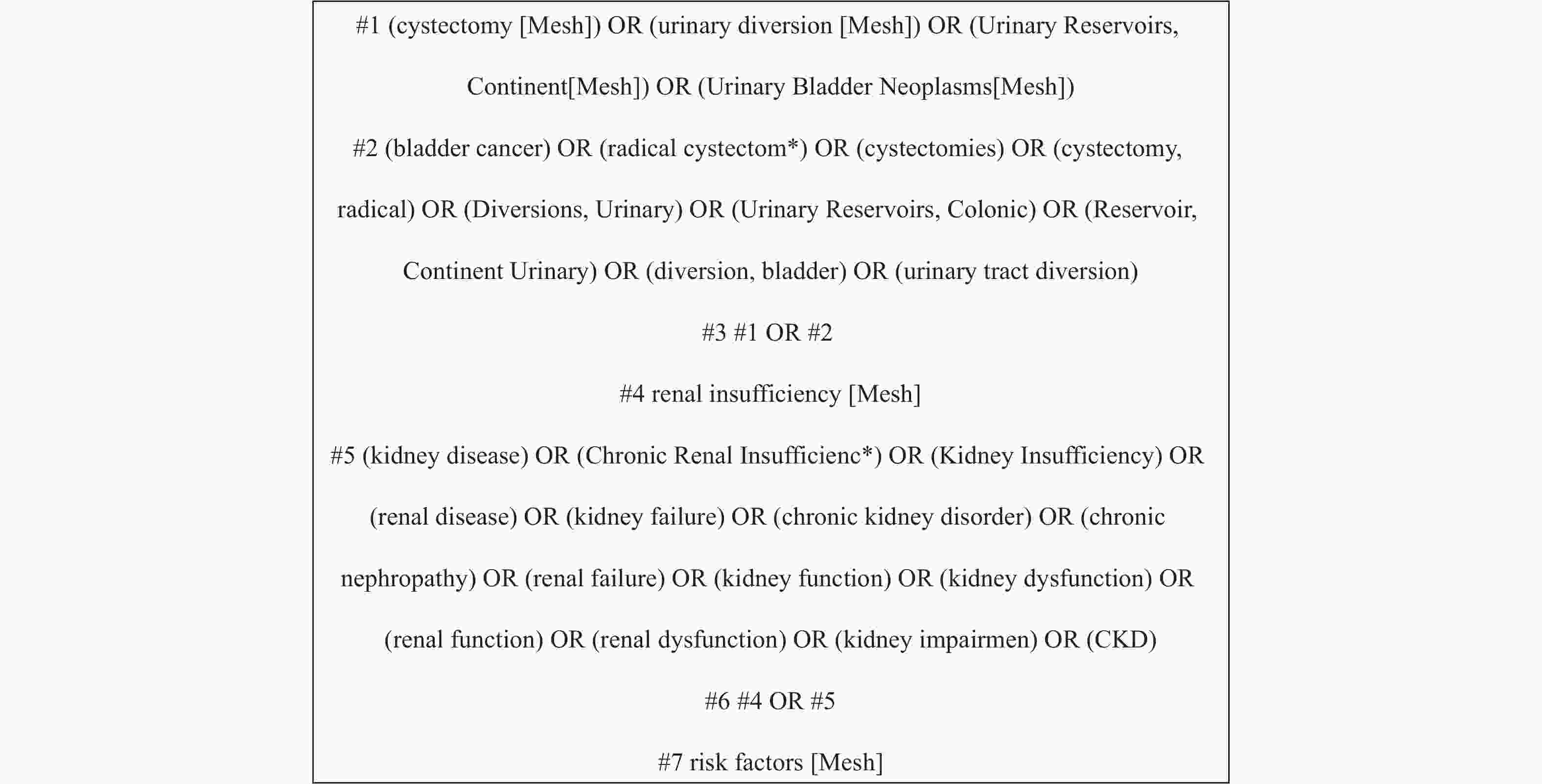
目的 系统评价根治性膀胱切除术患者术后肾功能损害的发生率及影响因素。 方法 检索维普、万方、中国知网、中国生物医学文献数据库、The Cochrane Library、PubMed、Web of Science和Embase数据库中与根治性膀胱切除术患者术后肾功能损害有关的队列研究与病例对照研究。检索时限为建库至2023年9月30日。由2名研究者按照纳入与排除标准独立进行文献筛选、文章质量评价并数据进行提取。采用Stata14.0软件对文献进行Meta分析。 结果 共纳入11篇文献,Meta分析显示,纳入研究的异质性较大(I 2 = 92.5%,P < 0.001),基于随机效应模型得出根治性膀胱切除术后患者肾功能损害发生率为32%[95%CI (0.25,0.35),P < 0.001],亚组分析显示,研究时长在5 a及其以上30%[95%CI (0.24,0.37),P < 0.001]、研究地区为亚洲35%[95%CI (0.28,0.42),P < 0.001]、以术后估计肾小球滤过率<45 mL/(min·1.73 m2)为评价肾功能损害的标准33%[95%CI (0.29,0.36),P < 0.001]、队列研究39%[95%CI (0.26,0.52),P < 0.001]肾功能损害发生率更高。术后发生肾功能损害的影响因素为年龄[HR = 1.03,95%CI (1.02,1.04)]、高血压[HR = 2.14,95%CI (1.32,3.40)]、肾积水[HR = 1.89,95%CI (1.50,2.36)]、尿路感染[HR = 1.35,95%CI (1.13,1.61)]和吻合口狭窄[HR = 2.53,95%CI (1.77,3.61)]。 结论 根治性膀胱切除术后肾功能损害发生率较高,且与年龄、高血压病史、术后肾积水、尿路感染及吻合口狭窄密切相关,医护人员应加强对此类患者术后肾功能的监测,针对相关影响因素制定有效措施,以降低肾功能损害的发生率。 Abstract:Objective To systematically evaluate the incidence and influencing factors of postoperative renal dysfunction in patients undergoing radical cystectomy. Methods The cohort studies and case-control studies related to postoperative renal function damage of patients undergoing radical cystectomy were retrieved from China HowNet, VIP, Wanfang, China Biomedical Literature Database, The Cochrane Library, PubMed, Web of Science and Embasedatabases. The retrieval time is from the establishment of the database to September 30, 2023. Two researchers independently conducted literature screening and article quality assessment based on predefined inclusion and exclusion criteria. Mata analysis was carried out on the literature with Stata14.0 software. Results A total of 11 articles were included. Meta-analysis showed that the heterogeneity of the included studies was large (I 2 = 92.5%, P < 0.001). Based on the random effect model, the incidence of renal function damage after radical cystectomy was 32%[95%CI (0.25, 0.35), P < 0.001], and subgroup analysis showed that the research duration was 5 years or more 30%[95%CI (0.24, 0.37), P < 0.001], the study area was Asia35%[95%CI (0.28, 0.42) in Asia, P < 0.001] , the postoperative estimated glomerular filtration rate was < 45 mL/(min·1.73m2) as the evaluation standard of renal function damage 33%[95%CI (0.29, 0.36), P < 0.001]and cohort studies 39%[95%CI (0.26, 0.52), P < 0.001]is higher. The influencing factors of postoperative renal dysfunction were age[HR = 1.03, 95%CI (1.02, 1.04)], hypertension [HR = 2.14, 95%CI (1.32, 3.40)], hydronephrosis [HR = 1.89, 95%CI (1.50, 2.36)], urinary tract infection[HR = 1.35, 95%CI (1.13, 1.61)] and Anastomotic stenosis [HR = 2.53, 95%CI (1.77, 3.61)]. Conclusion The incidence of renal function damage after radical cystectomy is high, which is closely related to age, history of hypertension, postoperative hydronephrosis, urinary tract infection and anastomotic stenosis. Medical staff should strengthen the monitoring of postoperative renal function and formulate effective measures for related influencing factors to reduce the incidence of renal function damage. -
Key words:
- Renal function damage /
- Radical cystectomy /
- Influencing factors /
- Systematic review /
- Meta analysis
-
表 1 纳入研究的基本特征及方法学质量评价(n = 11)
Table 1. Basic characteristics of the included studies and methodological quality assessment (n = 11)
纳入研究 国家 研究设计 样本量/中位
随访时间(月)尿流改道方式 结局指标
[mL/(min·1.73m2)]肾功能损伤
发生率(%)影响因素 NOS评分 陈少豪等
2017[9]中国 病例对照 156/89
(60~130)35.9%ONB,43.6%IC,
20.5%CU双肾总eGFR
下降≥25%41.70 ③⑤⑦ 7 Ahmadi等
2022[10]美国 病例对照 508/44
(11~85)/ eGFR下降≥10% 12.60 ①④⑨ 7 Elsayed等
2020[11]美国 病例对照 442/25
(12~59)87%IC,13%其他 术后eGFR< 45 37.10 ③④⑥⑦
⑫⑬⑮7 Eisenberg等
2014[12]美国 病例对照 1631 /126
(85~183)23%ONB,76%IC,
1%CUeGFR下降≥10% 27.00 ①④⑤
⑩⑫⑥7 Nishikawa等
2014[13]日本 队列研究 169/103.8±9.8 24.8%CU,23.7%IC,
51.5%ONB双肾总eGFR
下降≥25%46.20 ⑤⑥⑩ 7 Gershman等
2015[14]美国 队列研究 1383 /12073.8%IC,18.7%ONB,
7.5%其他eGFR下降≥10% / ①⑤⑩
⑪⑫7 郑玮等
2018[15]中国 病例对照 103/16
(3~36)48.5%ONB,23.3%IC,
28.2%CU术后eGFR< 60 38.90 ②④⑧ 7 Hatakeyama
等2016[16]日本 病例对照 115/97
(70~125)59.1%ONB,14.8%IU,
26.1%CU术后eGFR< 45 32.20 ①②④⑩ 7 Kwon等
2016[17]韩国 病例对照 866/
49.8
(1~231.4)/ 术后eGFR< 60 25.60 ①④⑨⑬ 8 Lone等
2021[18]美国 队列研究 644/32
(12~56)72%IC,17%ONB,
11%其他术后eGFR< 45 33.00 ④⑪⑫ 7 金滨等
2023[19]中国 病例对照 46/20
(12~67)45.7%IC,54.3%CU 双肾总eGFR
下降≥25%39.10 ⑥⑯ 7 注:影响因素:①年龄;②尿流改道方式;③糖尿病;④术前肾功能;⑤高血压;⑥尿路感染;⑦身体质量指数(body mass index,BMI);⑧术后早期肾功能(术后30 d内eGFR);⑨化疗;⑩术后肾积水;⑪肿瘤分期;⑫吻合口狭窄;⑬急性肾损伤;⑭吻合口狭窄;⑮放疗;⑯围手术期输血缩略式:输尿管皮肤造口(cutaneous ureterostomy,CU);回肠膀胱术(ileal conduit,IC);原位新膀胱(orthotopic neobladder,ONB);开放式根治性膀胱切除术(open radical cystectomy,ORC);机器人辅助腹腔镜根治性膀胱切除术(robotic-assisted radical cystectomy,RARC)。 表 2 根治性膀胱切除术后肾功能损害亚组分析结果
Table 2. Subgroup analysis of renal impairment after radical cystectomy
亚组 纳入研究(项) 异质性检验结果 效应模型 Meta分析结果 I 2(%) P 患病率(%) 95%CI P 研究时长 1 a[12,15,19] 3 70.4 0.034* 随机效应 33 [0.24,0.43] <0.001* 5 a及其以上[9−13,16−18] 7 94.7 <0.001* 随机效应 35 [0.29,0.41] <0.001* 地区 亚洲[9,13,15−17,19] 6 86.5 <0.001* 随机效应 37 [0.28,0.45] <0.001* 欧美[10−12,18] 4 96.1 <0.001* 随机效应 27 [0.19,0.36] <0.001* 结局指标
[mL/(min·1.73m2)]eGFR下降≥25%[9,13,16,19] 4 55.9 0.078 随机效应 40 [0.36,0.45] <0.001* 术后eGFR下降≥10% [10−12] 3 96.9 <0.001* 随机效应 26 [0.24,0.28] <0.001* 术后eGFR<60 [15,17] 2 79.7 <0.001* 随机效应 27 [0.24,0.30] <0.001* 术后eGFR<45 [18] 1 33 [0.29,0.36] <0.001* 研究设计 病例对照[9−12,15−17,19] 8 92.0 <0.001* 随机效应 29 [0.23,0.35] <0.001* 队列研究[13,18] 2 90.1 0.001* 随机效应 39 [0.26,0.52] <0.001* *P < 0.05。 表 3 根治性膀胱切除术后肾功能损害影响因素的Meta分析
Table 3. Meta-analysis of influencing factors of renal impairment after radical cystectomy
影响因素 纳入文献(项) 异质性检验结果 效应模型 Meta分析结果 I 2(%) P OR 95%CI P 年龄[10,12,14,16-17] 5 9.3 0.353 固定效应 1.03 [1.02,1.04] <0.001* 高血压[9,12−14] 4 71.9 0.014* 随机效应 1.70 [1.17,2.47] 0.005* 术前eGFR[10−12,15−18] 7 98.3 <0.001* 随机效应 0.99 [0.93,1.05] 0.660 肾积水[11−14,16] 5 74.5 0.004* 随机效应 1.84 [1.28,2.36] 0.001* 尿路感染[11−13,19] 4 79.4 0.002* 随机效应 2.34 [1.20,4.59] 0.013* 吻合口狭窄[11-12,14,18] 3 73.3 0.011* 随机效应 2.20 [1.55,3.12] <0.001* *P < 0.05。 表 4 根治性膀胱切除术后肾功能损害影响因素的Meta分析(剔除异质性来源后)
Table 4. Meta-analysis of factors influencing renal impairment after radical cystectomy (after exclusion of sources of heterogeneity)
影响因素 纳入文献(项) 异质性检验结果 效应模型 Meta分析结果 I 2(%) P OR 95%CI P 年龄[10,12,14,16,17] 5 9.3 0.353 固定效应 1.03 [1.02,1.04] <0.001* 高血压[9,13-14] 3 47.1 0.150 固定效应 2.14 [1.32,3.40] 0.002* 术前eGFR[10−12,15−18] 7 98.3 <0.001* 随机效应 0.99 [0.93,1.05] 0.660 肾积水[11,13−14,16] 4 48.4 0.121 固定效应 1.89 [1.50,2.36] <0.001* 尿路感染[11−12,19] 3 31.0 0.229 固定效应 1.35 [1.13,1.61] <0.001* 吻合口狭窄[11−12,14,18] 3 49.1 0.14 固定效应 2.53 [1.77,3.61] <0.001* *P < 0.05。 -
[1] Vejlgaard M,Maibom S,Stroomgerg H,et al. Long-term renal function following radical cystectomy for bladder cancer[J]. Urology,2022,160:147-153. doi: 10.1016/j.urology.2021.11.015 [2] 中国国家癌症中心. 膀胱癌诊疗指南(2022年版)[EB/OL]. (2022-04-11)[2024-01-12]. https://m.medlive.cn/guide/1/25548. [3] Amini E,Djaladat H. Long-term complications of urinary diversion[J]. Curr Opin Urol,2015,25(6):570-577. doi: 10.1097/MOU.0000000000000222 [4] Minguez O C,Artiles M A,Sanchez G A,et al. The impact of radical cystectomy on renal function: Identification of risk factors for development of chronic kidney disease[J]. European Urology Open Science,2022,45(2):S258-S259. doi: 10.1016/S2666-1683(22)02594-0 [5] Twrakawa T,Hussein A,May P,et al. Change in renal functions and risk of chronic kidney disease after robot-assisted radical cystectomy and urinary diversion[J]. Journal of Urology,2018,199(4):e878. [6] Chen J,Budoff M J,Reilly M P,et al. Coronary artery calcification and risk of cardiovascular disease and death among patients with chronic kidney disease[J]. Jama Cardiology,2017,2(6):635-643. doi: 10.1001/jamacardio.2017.0363 [7] 付帅,李晓宁. 肾小球滤过率计算公式研究进展: 从Cockcroft-Gault公式到FAS公式[J]. 临床肾脏病杂志,2020,20(1):73-77. [8] 曾宪涛,刘慧,陈曦,等. Meta分析系列之四: 观察性研究的质量评价工具[J]. 中国循证心血管医学杂志,2012,4(4):297-279. [9] 陈少豪,于翔,吴宇鹏,等. 根治性膀胱切除及尿流改道术后长期肾功能损害影响因素分析[J]. 临床泌尿外科杂志,2017,32(10):755-759. [10] Ahmadi H,Reddy S,Nguyen C,et al. Long-term renal function in patients with chronic kidney disease following radical cystectomy and orthotopic neobladder[J]. BJU Int,2022,130(2):200-207. doi: 10.1111/bju.15685 [11] Elsayed A,Jing Z,Demirbas D,et al. Development and cross-validation of a Nomogram for chronic kidney disease following robot-assisted radical cystectomy[J]. J Endourol,2020,34(9):946-954. doi: 10.1089/end.2020.0451 [12] Eisenberg S,Thompson R,Frank I,et al. Long-term renal function outcomes after radical cystectomy[J]. Journal of Urology,2014,191(3):619-625. doi: 10.1016/j.juro.2013.09.011 [13] Nishikawam,Miyake H,fujisawa M. Long-term observation of changes in renal function followingradical cystectomy and urinary diversion[J]. European Urology,Supplements,2014,13(1):1105-1111. [14] Gershman B,Eisenberg M,Thompson R,et al. Comparative impact of continent and incontinent urinary diversion on long-term renal function after radical cystectomy in patients with preoperative chronic kidney disease 2 and chronic kidney disease 3a[J]. Int J Urol,2015,22(7):651-656. [15] 郑玮,黄新冕,王帅,等. 机器人辅助腹腔镜膀胱癌根治术后肾功能改变的观察[J]. 临床泌尿外科杂志,2018,33(11):874-878,882. [16] Hatakeyama S,Koie T,Narita T,et al. Renal function outcomes and risk factors for stage 3B chronic kidney disease after urinary diversion in patients with muscle invasive bladder cancer[J]. PLoS One,2016,11(2):544. [17] Kwon T,Jeongig,Lee C,et al. Acute kidney injury after radical cystectomy for bladder cancer is associated with chronic kidney disease and mortality[J]. Annals of Surgical Oncology,2016,23(2):686-693. doi: 10.1245/s10434-015-4886-4 [18] Lone Z,Murthy P,Zhang H,et al. Comparison of renal function after open radical cystectomy,extracorporeal robot assisted radical cystectomy,and intracorporeal robot assisted radical cystectomy[J]. Urologic Oncology-Seminars and Original Investigations,2021,39(5):1-9. [19] 金滨,吕政通,敬吉波,等. 根治性膀胱全切术后不同尿流改道方式的并发症比较和肾功能 下降影响因素分析[J]. 中华老年医学杂志,2023,42(7):815-820. [20] Delanaye P,Gama R M,Clery A,et al. Estimated glomerular filtration rate equations in people of self-reported black ethnicity in the United Kingdom: Inappropriate adjustment for ethnicity may lead to reduced access to care[J]. PLoS One,2021,16(8):1-18. doi: 10.1371/journal.pone.0255869 [21] Gama R,Javeria P,Kate B,et al. Removal of ethnicity adjustment for creatinine-based estimated glomerular filtration rate equations[J]. Annals of Clinical Biochemistry: International Journal of Laboratory Medicine,2023,61(1):8-18. [22] Naganuma T,Takemoto Y,Maeda S,et al. Chronic kidney disease in patients with ileal conduit urinary diversion[J]. Exp Ther Med,2012,4(6):962-966. doi: 10.3892/etm.2012.703 [23] Todenhofer T,Stenzl A,Schwentner C. Optimal use and outcomes of orthotopic neobladder reconstruction in men and women[J]. Curr Opin Urol,2013,23(5):479-486. doi: 10.1097/MOU.0b013e328363f6e9 [24] Osman Y,Harraz A ,Halwagy S,et al. Acute kidney injury following radical cystectomy and urinary diversion: predictors and associated morbidity [J]. Int Braz J Urol,2018,44(4): 726-733. [25] 于书慧,丁光璞,李学松,等. 医护协作型原位新膀胱患者综合管理门诊的建立及实践效果[J]. 中国实用护理杂志,2021,37(36):2848-2852. doi: 10.3760/cma.j.cn211501-20201204-04725 [26] 陈玉,李娟,胡英娜,等. 基于行动研究的尿路造口周围刺激性皮炎护理方案的改进与实 施[J]. 中国护理管理,2023,23(4):486-490. doi: 10.3969/j.issn.1672-1756.2023.04.002 [27] Liu Z,Zhang B,Hu Y,et al. The cause analysis of benign uretero-ileal anastomotic stricture after radical cystectomy and urinary diversion[J]. Front Oncol,2022,12:1070-1074. -





 下载:
下载: