Factors Influencing the Development of Extra-Pulmonary Tuberculosis in Patients with Viral Hepatitis Complicated by Pulmonary Tuberculosis
-
摘要:
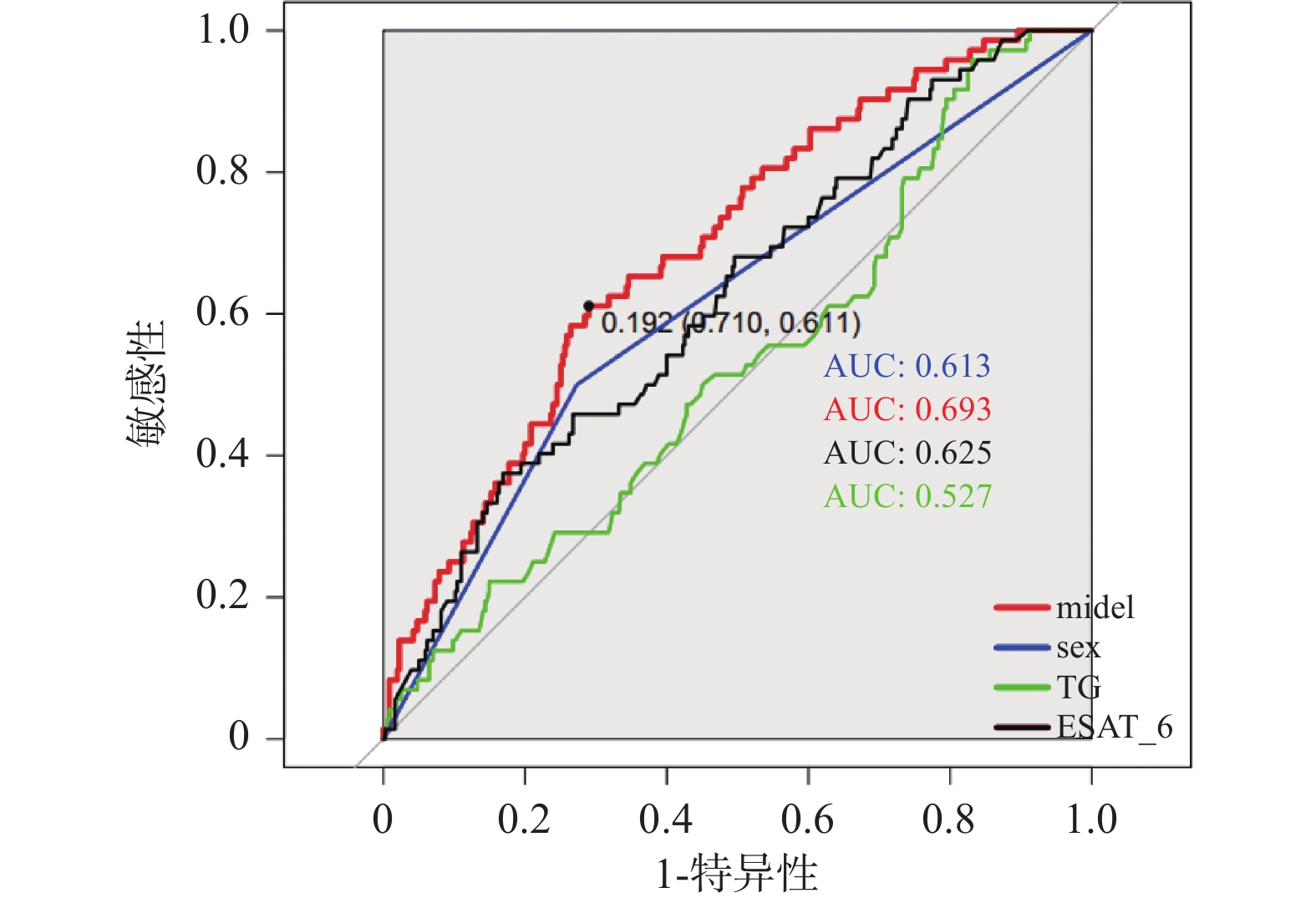
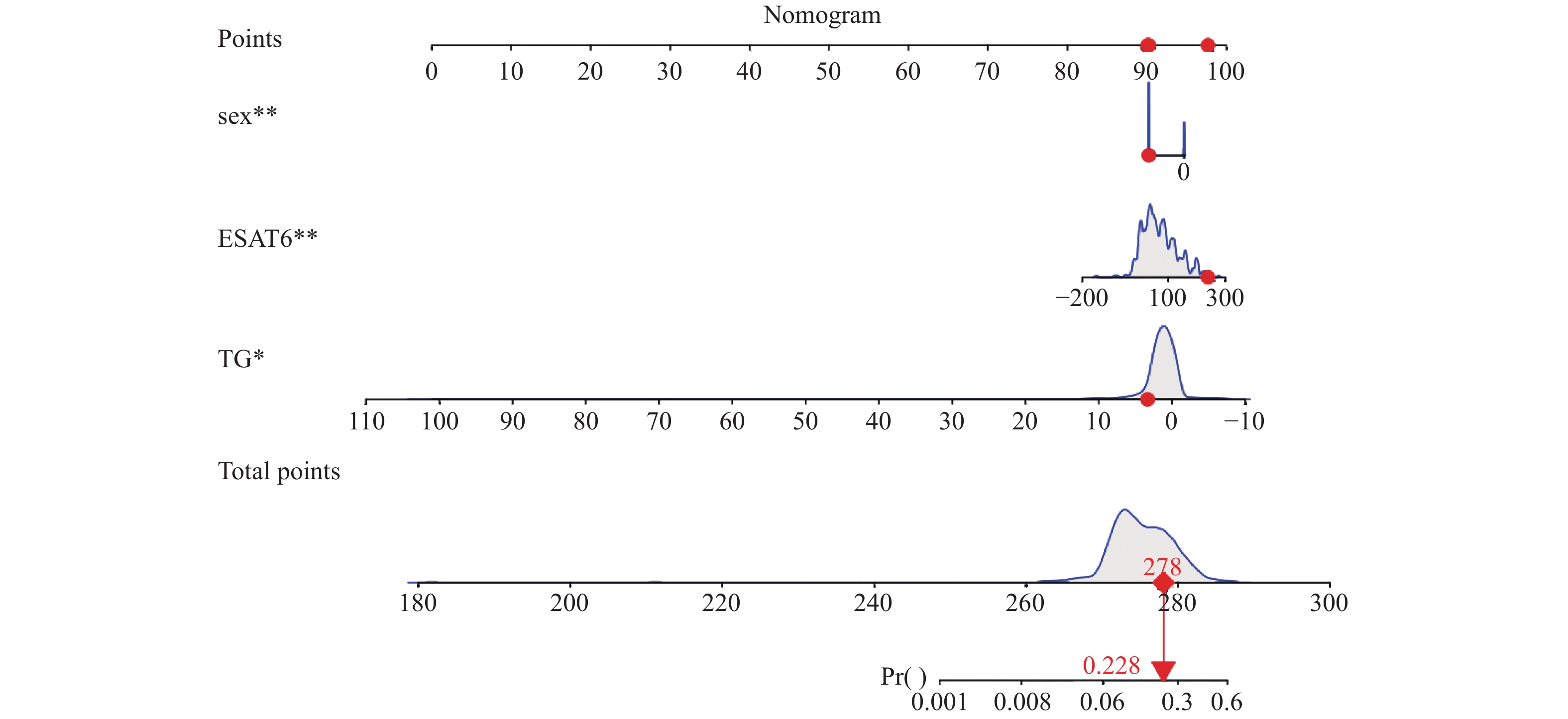
目的 探讨病毒性肝炎合并肺结核患者并发肺外结核(extra-pulmonary tuberculosis,EPTB)的影响因素。 方法 回顾分析昆明市第三人民医院2015年1月至2020年12月结核科收治的病毒性肝炎乙型(hepatitis B virus,HBV)和病毒性肝炎丙型(hepatitis C virus,HCV)合并肺结核(pulmonary tuberculosis,PTB)的患者427例,以是否并发EPTB分为并发EPTB组(n = 72)和未并发EPTB组(n = 355)。收集患者的临床资料,采用单因素、多因素Logistic回归筛选并发EPTB的独立危险因素作为预测因子,建立病毒性肝炎合并PTB患者并发EPTB的列线图预测模型,选用Hosmer-Lemeshow检验、ROC曲线评价。 结果 427名患者中男292例(68.3%),女135例(31.7%),并发EPTB72例,发生率16.86%。其中,EPTB中男34例(47.2%),女38例(52.8%),结核性胸膜炎21例(29%),结核性腹膜炎16例(22%),淋巴结结核13例(18%),结核性脑炎5例(6%),肠结核6例(8%),骨结核5例(6%),盆腔结核3例(4%)泌尿系统结核3例(4%)。多因素Logistic回归示,性别(OR = 0.425,95%CI:0.250~0.722,P = 0.02)、低水平甘油三脂(TG)(OR = 0.837,95%CI:0.717~0.978,P = 0.025)、结核特异性抗原A(ESAT-6)(OR = 1.007,95%CI:1.003~1.011是PTB合并HBV、HCV感染并发EPTB的独立影响因素。列线图模型的最佳截断值0.192,对应的灵敏度0.611、和特异度0.710、约登指数0.741、阳性似然比2.103、阴性似然比0.548。Hosmer-Lemeshow检验,χ2 = 2.631,P = 0.955。ROC曲线分析显示AUC:0.693,95%CI: 0.6291 ~0.7574 )。结论 基于性别、低水平TG、ESAT-6建立的预测模型能一定程度上预测是否并发EPTB,为临床治疗工作提供参考。 Abstract:Objective To investigate the factors influencing the development of extra-pulmonary tuberculosis (EPTB) in patients with viral hepatitis complicated by pulmonary tuberculosis(PTB). Methods A retrospective analysis was conducted on 427 patients with Hepatitis B Virus (HBV) and Hepatitis C Virus (HCV) infections complicated by PTB admitted to the tuberculosis department of Kunming Third People’ s Hospital from January 2015 to December 2020. Patients were divided into the EPTB complication group (n = 72) and the non-EPTB complication group (n = 355) based on the presence of EPTB.Clinical treatment data of patients were collected. Univariate and multivariate Logistic regression analyse were used to screen independent risk factors for EPTB as predictive factors. A nomogram prediction model was established for Extrapulmonary Tuberculosis (EPTB) complications in patients with viral hepatitis and Pulmonary Tuberculosis (PTB) , evaluated using the Hosmer-Lemeshow test and ROC curve analysis. Results Among the 427 patients, 292 (68.3%) were male and 135 (31.7%) were female, with 72 cases of EPTB, resulting in an incidence rate of 16.86%. In the EPTB group, there were 34 males (47.2%) and 38 females (52.8%). The types of EPTB included tuberculous pleuritis (21 cases, 29%), tuberculous peritonitis(16 cases, 22%), lymph node tuberculosis (13 cases, 18%), tuberculous encephalitis(5 cases, 6%), intestinal tuberculosis( 6 cases, 8%), bone tuberculosis(5 cases, 6%), pelvic tuberculosis(3 cases, 4%), and genitourinary tuberculosis(3 cases, 4%). Multivariate logistic regression analysis showed that gender (OR = 0.425, 95%CI: 0.250-0.722, P = 0.02), low triglyceride (TG) levels (OR = 0.837, 95%CI: 0.717-0.978, P = 0.025), the tuberculosis-specific antigen A (ESAT-6) (OR = 1.007, 95%CI: 1.003 ~ 1.011 were independent influencing factors for EPTB in patients with PTB complicated by HBV and HCV infections. The optimal cutoff value for the nomogram model is 0.192, with a sensitivity of 0.611, specificity of 0.710, Youden index of 0.741, positive likelihood ratio of 2.103, and negative likelihood ratio of 0.548. The Hosmer-Lemeshow test yielded χ2 = 2.631, P = 0.955. ROC curve analysis showed an AUC of 0.693, 95%CI: 0.6291 ~ 0.7574.Conclusion The prediction model based on gender, low TG levels and ESAT-6 can well predict the occurrence of EPTB to some extent, providing a reference for clinical treatment. -
结核病是结核杆菌(tubercle bacillus,TB)感染引起的全球性疾患,其发病率和死亡率均很高[1-2]。据《2022年全球结核病报告》[3],全球2021年约新增
1060 万人,其中,成年男性600万人,成年女性340万人,儿童120万人。病毒性肝炎是多种类型肝炎病毒引起的以肝脏损害为主表现的传染病,其中我国主要以乙型(hepatitis B virus,HBV)、丙型(hepatitis C virus,HCV)最常见,病毒性肝病和结核病均是我国公共卫生问题,它们危害人民身心健康、增加疾病负担。肺外结核(extra-pulmonary tuberculosis,EPTB)是指发生于肺部以外的其他脏器的结核病[4]。EPTB的治疗时间较肺结核(pulmonary tuberculosis,PTB)更长,病情更重,在合并病毒性肝炎这部分患者中更容易发生肝损害而导致停用抗结核药,产生的后果更容易对公共卫生造成严重的负担[5]。本研究回顾病毒性肝炎合并肺结核患者的临床资料,应用多因素Logistic回归筛选并发EPTB的独立危险因素作为预测因子,建立预测模型,为临床医师对病毒性肝炎合并肺外结核患者诊治提供参考。1. 资料与方法
1.1 研究对象
选取2015年1月至2020年12月在昆明市第三人民医院住院治疗,诊断为病毒性肝炎合并PTB的患者为研究对象,其中年龄最小者13岁,最大者81岁,且所有研究者均获得本人或监护人知情同意。本研究已通过昆明市第三人民医院伦理委员会审批通过(昆三伦:2022061615)。
1.2 纳入标准和排除标准
纳入标准:本研究病毒性肝炎患者包括HBV[6]和HCV[7]感染者。肺外结核诊断标准[8−9]:(1)组织病理示慢性肉芽肿,且qPCR找到TB核酸片段;(2)局部体液抗酸杆菌涂片阳性或培养出TB;(3)临床表现支持结核、排除其他疾病,且诊断性抗结核有效。肺结核诊断标准:满足《肺结核诊断标准》(WS288-2017)[10]。
排除标准:(1)非结核分支杆菌病;(2)HIV阳性、梅毒等传染病,合并自身免疫、疾病恶性肿瘤、重型心脑血管疾病者;(3)吸毒、长期大剂量激素、免疫制剂、生物制剂治疗患者。
1.3 样本量估算
目前文献中,缺乏病毒性肝炎并PTB患者中EPTB的发生率数据报导,为此,参考PTB并发EPTB的相关文献,进行样本量粗略计算。采用PASS2021软件,参数设置为a = 0.05(双侧检验),把握度 = 1-β = 0.8,结果为需要308例研究对象,再考虑10%的失访率,至少需要385例的研究对象,因目前缺乏研究对象的发生率数据,纳入了选取期间满足纳入标准的所有患者427例,满足需求,可保证研究的科学性。
1.4 数据收集
在昆明市第三人民医院信息系统中查阅病毒性肝炎合并PTB患者的住院资料,并收集其临床资料:包括年龄、性别、民族、临床症状、体征、体重指数(body mass index,BMI)及、谷氨酰转肽酶(glutamyl transpeptidas,GGT)、白蛋白(albumin,ALB)、血小板(platelet,PLT)、血清总胆红素(total bilirubin,TBIL)、白细胞(white blood cell,WBC)、淋巴细胞(lymphocyte,LYMP)、碱性磷酸酶(alkaline phosphatase,ALP)、红细胞(red blood cell,RBC)、中性粒细胞(neutrophils,NEUT)、血红蛋白(hemoglobin,HB)、谷丙转氨酶(alanine transaminase,ALT)、尿酸(uric acid,UA)、球蛋白(globulin,GLB)、CFP-10、谷草转氨酶(aspartate aminotransferase,AST)、肌酐(creatinine,Cr)、尿素氮(urea)、血沉(erythrocyte sedimentation rate,ESR)、甘油三酯(triglyceride,TG)、结核特异性抗原A(ESAT-6)等实验室资料。痰涂片采用萋-尼抗酸杆菌染色显微镜检,结核菌培养采用液体快速培养和罗氏固体培养,仪器分别为贝索和BD960,血常规采用XN-10自动血细胞分析仪,血生化采用AU680 Series自动生化分析仪。
1.5 统计学分析
将收集的数据建立Excel数据库,采用SPSS 26.0分析。计数资料采用率、构成比表示,非正态分布的计量资料采用M(P25,P75)表示,呈正态分布的计量资料采用均数±标准差($ \bar x \pm s $)。Logistic回归筛选出独立危险因素作为预测因子,R 4.23 和 RStudio
1.2.5042 中“rms”包拟合列线图预测模型。采用,Hosmer-Lemeshow检验和ROC曲线评价预测模型。P < 0.05为差异有统计学意义,检验水准α = 0.05,双侧检验。2. 结果
2.1 病毒性肝炎合并肺结核患者并发肺外结核的基本临床信息
2015年1月至2020年12月病毒性肝炎合并PTB的427名患者为研究对象,其中并发肺外结核的72例为并发EPTB组,其发生率为16.86%,包括结核性胸膜炎21例(29.0%),结核性腹膜炎16例(22.0%),淋巴结结核13例(18.0%),结核性脑炎5例(6.0%),肠结核6例(8.0%),骨结核5例(6.0%),盆腔结核3例(4.0%),泌尿系统结核3例(4.0%)。其中HCV感染患者15例(占20.8%)、HBV感染59例(占81.9%),男性34例(47.2%)、女性38例(52.8%),汉族59例(81.9%),年龄中位数43岁。仅合并PTB的355例为未并发EPTB组,包括HCV感染患者70例(占19.7%),HBV感染299例(占84.2%),其中男性258例(72.7%),女性97例(227.3%),汉族321例(90.4%),年龄中位数43岁,依据BMI体重过轻者16例(22.2%)、正常42例(58.3%)、超重14例(19.5%),出现发热12例(16.7%)。在并发与未并发EPTB比较中,性别、民族、HB、Cr、ESAT-6、CFP-10差异有统计学意义(P < 0.05),见表1。
表 1 并发与未并发肺外结核患者的临床特征比较[n(%)/M(P25,P75)]Table 1. Comparison of clinical characteristics between patients with and without extrapulmonary tuberculosis. [n(%)/M(P25,P75)]指标 并发EPTB(n = 72) 未并发EPTB组(n = 355) Z/χ2 P 性别(男) 34(47.2) 258(72.7) 17.938 < 0.001* 年龄 43(33.0~55.0) 43(30.0~55.0) −0.850 0.396 民族(汉) 59(81.9) 321(90.4) 4.392 0.036* 饮酒史 11(15.3) 66(18.6) 0.445 0.505 吸烟史 14(19.4) 81(22.8) 0.394 0.530 BMI (kg/m2) 体重过轻 16(22.2) 95(26.8) 正常 42(58.3) 216(60.8) −1.404 0.160 超重 14(14.5) 44(12.4) HCV 15(20.8) 70(19.7) 0.047 0.829 HBV 59(81.9) 299(84.2) 0.230 0.632 发热 12(16.7) 66(18.6) 0.149 0.700 WBC(109/L) 5.375(4.723~7.75) 5.74(4.5~7.1) −0.418 0.676 RBC(1012/L) 4.52(4.13~4.87) 4.58(4.15~5.07) −1.009 0.313 PLT(109/L) 226(169.00~304.75) 218(163.00~273.00) −1.690 0.091 HB(g/L) 133(115.00~141.00) 137(121.00~152.00) −2.269 0.023 TBIL(μmol/L) 11.05(7.33~18.38) 10.2(7.60~15.60) −0.897 0.370 Cr(μmol/L) 58.9(52~68.78) 64.1(55.3~75.6) −2.485 0.013* ALT(U/L) 22.5(11~36.45) 22(14.7~40) −0.748 0.455 AST(U/L) 23(17.25~39.5) 25(18~40) −0.892 0.372 ALB(g/L) 34.6(30.93~37.50) 36.1(32.2~39.41) −1.740 0.082 TG 0.945(0.655~1.482) 0.99(0.68~1.58) −0.729 0.466 ESAT-6 78.8(41~143) 55.2(22.16~103.4) −3.342 0.001* CFP-10 79.5(28.37~158.76) 56.54(13.5~126.96) −2.318 0.020* *P < 0.05。 2.2 并发肺外结核的影响因素分析
将研究指标进行单因素分析,P < 0.05者即性别、民族、PLT、TG、ESAT-6纳入多因素Logistic回归分析,结果显示:性别(OR = 0.425,95%CI:0.250~0.722,P = 0.02)、TG(OR = 0.837,95%CI:0.717~0.978,P = 0.025)、ESAT-6(OR = 1.007,95%CI:1.003~1.011)是病毒性肝炎合并PTB患者并EPTB的独立影响因素,见表2。
表 2 病毒性肝炎合并肺结核患者并发肺外结核的单因素分析Table 2. Univariate analysis of extrapulmonary tuberculosis in patients with viral hepatitis complicated by pulmonary tuberculosis变量 单因素二元Logistic回归 OR(95%CI) P BMI(kg/m2) 1.256(0.880~1.793) 0.209 性别 0.376(0.224~0.631) < 0.001* 年龄 0.993(0.976~1.010) 0.399 民族 2.080(1.036~4.176) 0.039* 饮酒史 0.790(0.394~1.583) 0.506 吸烟史 0.801(0.448~1.435) 0.456 乙肝 0.681(0.392~1.183) 0.172 丙肝 1.689(0.974~2.927) 0.062 发热 0.906(0.406~1.782) 0.774 WBC(109/L) 0.993(0.980~1.109) 0.906 NEUT(%) 1.008(0.989~1.028) 0.405 PLT(109/L) 1.002(1.000~1.004) 0.030* HB(g/L) 0.942(0.982~1.001) 0.097 RBC(1012/L) 0.942(0.789~1.126) 0.513 TBIL(μmol/L) 1.071(0.989~1.026) 0.464 Cr (μmol/L) 0.993(0.980~1.006) 0.309 ALT(U/L) 0.998(0.994~1.003) 0.489 AST(U/L) 0.998(0.991~1.005) 0.568 ALB(g/L) 0.983(0.946~1.022) 0.396 TG 0.829(0.714~0.963) 0.014* ESAT-6 1.007(1.003~1.011) < 0.001* CFP-10 1.002(0.999~1.004) 0.161 *P < 0.05。 2.3 评价三者联合对并发肺外结核的预测价值
绘ROC曲线,见图1,三者联合的预测效能为:AUC:0.693,95%CI:
0.6291 ~0.7574 ),其中最佳截断值0.192,对应的灵敏度和特异度分别为0.611、0.710,阳性似然比和阴性似然比分别为:2.103、0.548,见表3。表 3 性别、TG、ESAT-6及model预测并发EPTB的ROC曲线分析Table 3. ROC curve analysis for sex,TG,ESAT-6,and model for predicting concomitant extrapulmonary tuberculosis (EPTB)检验变量 AUC(95%CI) 最佳截断值 灵敏度(%) 特异度(%) 约登指数 阳性似然比 阴性似然比 P 性别 0.613(0.551~0.676) - 50.0 72.7 0.227 1.831 0.678 0.002* TG 0.527(0.455~0.599) 2.025 95.8 16.9 0.127 1.153 0.248 0.466 ESAT-6 0.625(0.555~0.695) 119.278 37.5 83.1 0.206 2.217 0.752 0.001* 模型 0.693(0.629~0.757) 0.192 61.1 71.0 0.741 2.103 0.548 < 0.001* *P < 0.05。 2.4 列线图呈现预测模
以性别、TG、ESAT-6这3个并发EPTB的独立危险因素作为预测因子,基于二元logistic回归方程,运用RStudio拟合预测模型,以列线图呈现所建立的预测模型,见图2。
3. 讨论
3.1 病毒性肝炎合并肺结核患者并发EPTB的构成分析
有研究表明,EPTB占结核患者的21.8%,结核性脑炎和结核性胸膜炎是EPTB最常见的形式[11]。中国以往的报告显示,EPTB占结核病人口的31.3%,常见的EPTB形式是骨结核和结核性胸膜炎。据国内多中心研究报道,PTB患者合并EPTB的并发率为11.93%,并发率依次为结核性脑膜炎2.72%、颈部淋巴结结核1.93%[12]。本研究结果表明,病毒性肝炎并肺结核患者EPTB的并发率为16.86%,其并发率高于普通人群,考虑这类患者肝脏合成能力下降,白蛋白合成降低,机体免疫下降,结核杆菌更容易在肺外组织、器官活动。此外,笔者的研究中,EPTB占比最高的是结核性胸膜炎为29%,在PTB合并病毒性肝炎这部分患者中结核性胸膜炎是发病率最高的,与之前的报道稍有不同,分析原因:(1)结核为慢性消耗性疾病,容易出现前白蛋白、白蛋白减少,免疫降低,而肝炎患者同样容易产生低蛋白血症、免疫功能下降,免疫功能下降是结核性胸膜炎的危险因素,同时低蛋白血症容易形成胸腔积液;(2)胸膜应对结核分枝杆菌分泌的毒素时产生强烈的炎症反应、免疫损伤。因此,有胸腔积液的病毒性肝炎合并肺结核的患者应重点进行鉴别诊断,以适时延长抗结核疗程为9~12个月让患者获益。
3.2 性别、TG、ESAT-6在并发EPTB中的临床价值分析
对病毒性肝炎合并PTB的患者收集到的人口学特征、实验室指标等进行统计学分析,单因素及多因素分析,结果显示性别、TG、ESAT-6是并发EPTB的独立影响因素(P < 0.05)。陈伟[13]教授指出,EPTB发病率男性高于女性,考虑因男性外出务工结核分枝杆菌感染的机会更大,在过度劳累、免疫力低下时容易发病。也有研究[14−15]发现,女性是患EPTB的独立危险因素,在中国香港进行的一项对
5747 名肺结核患者进行的横断面研究发现,女性EPTB的发病率高于男性,而男性肺结核发病率是高于女性。笔者发现,在病毒性肝炎合并肺结核患者中,女性并发EPTB的风险高于男性(OR = 0.425;95%CI:0.250~0.722),这与沙特阿拉伯[16]、土耳其[17]、尼泊尔[18]的研究一致。其机制可能是性别免疫二态性受性类固醇激素的调节,女性患者产生更强烈、更持久的免疫应答,和男性相比更不容易受到病毒感染,而女性更有效的抗病毒免疫防御会产生强烈的炎症反应[19]。病毒感染合并肺结核感染与单感染肺结核患者相比,这些患者的结核特异性IFN-γ+CD38+CD4+和IFN-γ+HLA-DR+CD4+ t细胞水平降低。这表明病毒感染合并肺结核感染这类人对结核的CD4+ t细胞免疫反应受损,在女性产生强烈炎症反应的时候更容易并发EPTB。为此,对病毒性肝炎合并PTB的女性患者需要密切关注CD4+ t的数值变化,其降低时需警惕EPTB的发生。甘油三酯(TG)、血清总胆固醇(TC)等脂类维持生命细胞基础代谢的必不可少的物质,也是TB感染期重要的能量物质。TB进入机体后,TB生长、繁殖、免疫逃逸等一系列过程与部分脂类代谢基因的表达密切相关。Chen等[20]发现,游离脂肪酸、TG、TC等脂类在PTB患者中表达有降低,然而TB治疗后又恢复正常,可能是由于肺结核患者脂类合成减少、代谢增加[21]。Matthew等[22]发现,PTB的肺部肉芽肿内的脂类含量明显增加。TG是干酪样坏死中的重要成分,是内源性能量和游离脂肪酸的储存物质,也是TB重要的营养物质[23],导致了PTB并发EPTB患者对TG消耗更多。笔者的研究发现高水平TG是EPTB的保护因素(OR = 0.834;95%CI:0.710-0.980),这也可说明EPTB患者需要更多的TG参与肉芽肿的形成,在多系统发生结核感染的时候需要消耗更多的甘油脂类物质,与文献报告的一致,在临床工作中可关注TG的变化情况,如TG水平较低者注意排查EPTB。
早期分泌性抗原(ESAT-6)是TB分泌的重要毒力因子之一,参与调控巨噬细胞自噬、凋亡、炎症激活等过程。其通过抑制机体巨噬细胞吞噬杀菌和自噬反应抵抗能力,减轻机体对TB的清除力,同时诱导巨噬细胞凋亡反应促进TB扩散定植,引起机体固有免疫防御受损、抗原提呈延迟[24]。本研究发现ESAT-6是病毒性肝炎合并肺结核并发肺外结核者的(OR = 1.007;95%CI:1.003~1.011)独立危险因素,TB感染机体后ESAT-6诱导的巨噬细胞的凋亡与固有免疫细胞的大量坏死促进TB的扩散、定植,引发TB的全身感染[25],ESAT-6也在积极抑制辅助T细胞的保护性免疫反应导致抑制相关促炎细胞因子的分泌,造成机体免疫紊乱,加速TB感染。
3.3 基于性别、TG、ESAT-6建立的模型预测并发EPTB的临床意义
本研究采用性别、TG、ESAT-6这三者联合预测病毒性肝炎合并肺结核患者并发EPTB的潜在风险并构建模型,可视化模型,具有实用性和科学性,使用ROC曲线进行了评价。在笔者的研究中,基于性别、TG、ESAT-6建立的预测模型的AUC:0.693,95%CI:
0.6291 ~0.7574 ),最佳截断值0.192,灵敏度0.611、特异度0.710、阳性似然比2.103、阴性似然比0.548。该模型预测性能一般,但目前国内外无相关模型报道,其能够在一定程度上帮助临床医师更加直观地预判此类人群并发EPTB的风险。国内外的文章报道PTB并发EPTB的较多,但是报道病毒性肝炎合并PTB患者并发EPTB的不多见。本研究发现女性、低水平TG、ESAT-6是其独立危险因素,不足之处在于小样本单中心研究,有待增大样本量多中心研究。 -
表 1 并发与未并发肺外结核患者的临床特征比较[n(%)/M(P25,P75)]
Table 1. Comparison of clinical characteristics between patients with and without extrapulmonary tuberculosis. [n(%)/M(P25,P75)]
指标 并发EPTB(n = 72) 未并发EPTB组(n = 355) Z/χ2 P 性别(男) 34(47.2) 258(72.7) 17.938 < 0.001* 年龄 43(33.0~55.0) 43(30.0~55.0) −0.850 0.396 民族(汉) 59(81.9) 321(90.4) 4.392 0.036* 饮酒史 11(15.3) 66(18.6) 0.445 0.505 吸烟史 14(19.4) 81(22.8) 0.394 0.530 BMI (kg/m2) 体重过轻 16(22.2) 95(26.8) 正常 42(58.3) 216(60.8) −1.404 0.160 超重 14(14.5) 44(12.4) HCV 15(20.8) 70(19.7) 0.047 0.829 HBV 59(81.9) 299(84.2) 0.230 0.632 发热 12(16.7) 66(18.6) 0.149 0.700 WBC(109/L) 5.375(4.723~7.75) 5.74(4.5~7.1) −0.418 0.676 RBC(1012/L) 4.52(4.13~4.87) 4.58(4.15~5.07) −1.009 0.313 PLT(109/L) 226(169.00~304.75) 218(163.00~273.00) −1.690 0.091 HB(g/L) 133(115.00~141.00) 137(121.00~152.00) −2.269 0.023 TBIL(μmol/L) 11.05(7.33~18.38) 10.2(7.60~15.60) −0.897 0.370 Cr(μmol/L) 58.9(52~68.78) 64.1(55.3~75.6) −2.485 0.013* ALT(U/L) 22.5(11~36.45) 22(14.7~40) −0.748 0.455 AST(U/L) 23(17.25~39.5) 25(18~40) −0.892 0.372 ALB(g/L) 34.6(30.93~37.50) 36.1(32.2~39.41) −1.740 0.082 TG 0.945(0.655~1.482) 0.99(0.68~1.58) −0.729 0.466 ESAT-6 78.8(41~143) 55.2(22.16~103.4) −3.342 0.001* CFP-10 79.5(28.37~158.76) 56.54(13.5~126.96) −2.318 0.020* *P < 0.05。 表 2 病毒性肝炎合并肺结核患者并发肺外结核的单因素分析
Table 2. Univariate analysis of extrapulmonary tuberculosis in patients with viral hepatitis complicated by pulmonary tuberculosis
变量 单因素二元Logistic回归 OR(95%CI) P BMI(kg/m2) 1.256(0.880~1.793) 0.209 性别 0.376(0.224~0.631) < 0.001* 年龄 0.993(0.976~1.010) 0.399 民族 2.080(1.036~4.176) 0.039* 饮酒史 0.790(0.394~1.583) 0.506 吸烟史 0.801(0.448~1.435) 0.456 乙肝 0.681(0.392~1.183) 0.172 丙肝 1.689(0.974~2.927) 0.062 发热 0.906(0.406~1.782) 0.774 WBC(109/L) 0.993(0.980~1.109) 0.906 NEUT(%) 1.008(0.989~1.028) 0.405 PLT(109/L) 1.002(1.000~1.004) 0.030* HB(g/L) 0.942(0.982~1.001) 0.097 RBC(1012/L) 0.942(0.789~1.126) 0.513 TBIL(μmol/L) 1.071(0.989~1.026) 0.464 Cr (μmol/L) 0.993(0.980~1.006) 0.309 ALT(U/L) 0.998(0.994~1.003) 0.489 AST(U/L) 0.998(0.991~1.005) 0.568 ALB(g/L) 0.983(0.946~1.022) 0.396 TG 0.829(0.714~0.963) 0.014* ESAT-6 1.007(1.003~1.011) < 0.001* CFP-10 1.002(0.999~1.004) 0.161 *P < 0.05。 表 3 性别、TG、ESAT-6及model预测并发EPTB的ROC曲线分析
Table 3. ROC curve analysis for sex,TG,ESAT-6,and model for predicting concomitant extrapulmonary tuberculosis (EPTB)
检验变量 AUC(95%CI) 最佳截断值 灵敏度(%) 特异度(%) 约登指数 阳性似然比 阴性似然比 P 性别 0.613(0.551~0.676) - 50.0 72.7 0.227 1.831 0.678 0.002* TG 0.527(0.455~0.599) 2.025 95.8 16.9 0.127 1.153 0.248 0.466 ESAT-6 0.625(0.555~0.695) 119.278 37.5 83.1 0.206 2.217 0.752 0.001* 模型 0.693(0.629~0.757) 0.192 61.1 71.0 0.741 2.103 0.548 < 0.001* *P < 0.05。 -
[1] Pai M,Behr M A,Dowdy D,et al. Tuberculosis[J]. Nat Rev Dis Primers,2016,2:16076. doi: 10.1038/nrdp.2016.76 [2] Furin J,Cox H,Pai M. Tuberculosis[J]. Lancet,2019,393(10181):1642-1656. doi: 10.1016/S0140-6736(19)30308-3 [3] World Health Organization. Global tuberculosis report 2022[Z/OL]. Geneva: World Health Organization,2022 [2023-10-29]. https://iris.who.int/handle/10665/363752. [4] 盛吉芳. 肺外结核[C]//第十次全国感染病学术会议暨第二届全国感染科医师大会、第四届中美临床微生物研讨会论文集. 杭州: 中华医学会感染病学分会,2008: 24-29. [5] Lee J Y. Diagnosis and treatment of extrapulmonary tuberculosis[J]. Tuberc Respir Dis (seoul),2015,78:47-55. doi: 10.4046/trd.2015.78.2.47 [6] 中华医学会感染病学分会,中华医学会肝病学分会. 慢性乙型肝炎防治指南(2019年版)[J]. 国际流行病学传染病学杂志,2019,46(6):423-446. [7] 中华医学会肝病学分会,中华医学会感染病学分会. 丙型肝炎防治指南(2022年版)[J]. 中华临床感染病杂志,2022,15(6):428-447. [8] 高亮,欧勤芳,赵新国. Gene Xpert在肺外结核病临床诊断中的价值探讨[J]. 热带医学杂志,2023,23(3):324-326+359. [9] 徐烨. T-SPOT. TB在肺外结核诊断中的应用价值研究[J]. 实验与检验医学,2019,37(3):528-530. doi: 10.3969/j.issn.1674-1129.2019.03.059 [10] 王黎霞, 成诗明, 周林, 等. 肺结核诊断WS288-2017[J]. 中国感染控制杂志,2018,17(7):642-652. [11] Pang Y ,An J,Shu W,et al (2019) Epidemiology of extrapulmonary tuberculosis among inpatients,China,2008–2017[J]. Emerg Infect Dis, 2019, 25(3): 457-464. [12] Wang X. Insight to the Epidemiology and Risk Factors of Extrapulmonary Tuberculosis in Tianjin,China during 2006-2011[J]. PLoS One.,2014,9(12):e112213. [13] 刘燕飞,李涛,夏愔愔,等. 2018-2020年9家结核病定点医院肺外结核病住院患者特征分析[J]. 疾病监测,2023,38(10):1223-1228. [14] Yang Z,Kong Y,Wilson F,et al. Identification of risk factors for extrapulmonary tuberculosis. Clin Infect Dis[J]. 2004, 38(2): 199-205. [15] Nisar M,Williams C S,Davies P D. Experience of tuberculosis in immigrants from South East Asia-implications for the imminent lease back of Hong Kong[J]. Respir Med.,1991,85(3):219-222. [16] Guler S A,Bozkus F,Inci M F,et al. Evaluation of pulmonaryand extrapulmomary tuberulosis in lmmunocompetentadults; a retrospective case series analysis[J]. Med PrincPract,2015,24(1):75-79. [17] Gunal S,Yang Z,Agarwal M, et al. Demographic and micro-bial characteristics of extrapultnonary tuberculosis cases diag-nosed in Malatya,Turkey,2001—2007[J]. BMC Public Health,2011,11;154. [18] Sreeramareddy C T,Panduru K V,Verma S C,et al. Compari-son of pulmonary and extrapulmonary tuberculosis in Nepal-ahospital-based retrospective study[J]. BMC Infect Dis,2008,8:8. doi: 10.1186/1471-2334-8-8 [19] Ruggieri A,Gagliardi M C,Anticoli S. Sex-dependent outcome of hepatitis B and C viruses infections: Synergy of sex hormones and immune responses? Front Immunol[J]. 2018, 9: 2302. [20] Chen J X,Han Y S,Zhang S Q,Li Z B,Chen J,Yi W J,et al. Novel therapeutic evaluation biomarkers of lipid metabolism targets in uncomplicated pulmonary tuberculosis patients[J]. Signal Transduction and Targeted Therapy,2021,6(1):22. doi: 10.1038/s41392-020-00427-w [21] 董娜,付玉荣,伊正君. 结核分枝杆菌感染致脂代谢异常及其机制研究进展[J]. 中华结核和呼吸杂志,2016,39(7):548-550. [22] Wipperman M F,Sampson N S,Thomas S T. Pathogen roid rage: cholesterol utilization by Mycobacterium tuberculosis[J]. Critical Reviews in Biochemistry and Molecular Biology,2014,49(4):269-293. [23] Alvarez H M. Triacylglycerol and wax ester-accumulating machinery inprokaryotes[J]. Biochimie,2016,120:28-39. doi: 10.1016/j.biochi.2015.08.016 [24] Belogorodtsev S N,Nemkova E K,Stavitskaya N V,et al. Pathogenic effects of M. tuberculosis-specific proteins ESAT-6 and CFP-10 in macrophage culture and in 3D-granulemogenesis model in vitro[J]. Bull Exp Biol Med,2021,171(5):656-660. [25] 李玉洁,余海燕,杨雨婷,等. 结核分枝杆菌分泌蛋白早期分泌性抗原6(ESAT-6)的免疫学性质及其在新型疫苗中作用的研究进展[J]. 细胞与分子免疫学杂志,2024,40(1):89-94. -






 下载:
下载:
 下载:
下载:

